SUMMARY: Bone is the most common site of metastatic disease, in patients with Breast Cancer. Bisphosphonates inhibit osteoclast-mediated bone resorption and both oral and IV bisphosphonates reduce the risk of developing Skeletal Related Events (SRE’s) and delay the time to SRE’s in patients with Breast Cancer with bone metastases. Bisphosphonates can also reduce bone pain and may improve Quality of life. Of the four bisphosphonates proven to be effective in patients with Breast Cancer with bone metastases, only intravenous Pamidronate (AREDIA®) and Zoledronic acid (ZOMETA®) have been approved in the USA, whereas intravenous and oral Ibandronate and oral Clodronate have been approved in Europe. Both AREDIA® and ZOMETA® are administered every 3 to 4 weeks during the first year, following diagnoses of bone metastases. However, the optimal treatment schedule following this initial phase of treatment has remained unclear. Further, renal toxicity, long bone fractures and OsteoNecrosis of the Jaw (ONJ) have been identified as potential problems with bisphosphonate use. OPTIMIZE-2 is a prospective, randomized, double-blind, multicenter trial, in which the authors evaluated the outcomes of a less intense schedule of ZOMETA® administered every 12 weeks, following one year of the standard initial phase of treatment with bisphosphonates. This study included 403 women with bone metastases from Breast Cancer, who had received 9 or more doses of either intravenous ZOMETA® or AREDIA®, during the first 10-15 months of therapy. The median age was 59 years and patients were randomized (1:1) to receive either ZOMETA® 4 mg IV every 4 weeks (N=200) or every 12 weeks (N=203), for one year. The primary endpoint was Skeletal Related Event (SRE) rate, defined as the proportion of patients with one or more SRE’s (pathologic fractures, spinal cord compression, need for radiotherapy or surgical stabilization of the bone). The primary analysis was non-inferiority, for the difference in SRE rates between the treatment groups. Secondary endpoints included time to first SRE, Skeletal Morbidity Rate (SMR), bone pain score, change in bone turnover markers, and safety. After a median follow up of 11.9 months, the SRE rate was 22% and 23.2% in the ZOMETA® every 4 weeks group and ZOMETA® every 12 weeks group respectively (P=0.724), suggesting that ZOMETA® given every 12 weeks was non-inferior to the q 4 week regimen. The secondary endpoints were comparable as well. More patients had renal toxicities in the ZOMETA® q 4 week group vs q 12 week group (9.6% vs 7.9%, respectively) and two cases (1.0%) of OsteoNecrosis of the Jaw (ONJ) were reported in the ZOMETA® q 4 week group. The authors concluded that the efficacy of continuing ZOMETA® for an additional year at the q 12 week schedule was non-inferior to ZOMETA® given q 4 weeks, among patients who had initially received IV bisphosphonates monthly, for one year or longer. Further the less frequent dosing of ZOMETA® compared with the standard monthly dosing, may be more convenient for the patients and result in less toxicities. Hortobagyi GN, Lipton A, Chew HK, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA9500)
OPTIMIZE-2 is a prospective, randomized, double-blind, multicenter trial, in which the authors evaluated the outcomes of a less intense schedule of ZOMETA® administered every 12 weeks, following one year of the standard initial phase of treatment with bisphosphonates. This study included 403 women with bone metastases from Breast Cancer, who had received 9 or more doses of either intravenous ZOMETA® or AREDIA®, during the first 10-15 months of therapy. The median age was 59 years and patients were randomized (1:1) to receive either ZOMETA® 4 mg IV every 4 weeks (N=200) or every 12 weeks (N=203), for one year. The primary endpoint was Skeletal Related Event (SRE) rate, defined as the proportion of patients with one or more SRE’s (pathologic fractures, spinal cord compression, need for radiotherapy or surgical stabilization of the bone). The primary analysis was non-inferiority, for the difference in SRE rates between the treatment groups. Secondary endpoints included time to first SRE, Skeletal Morbidity Rate (SMR), bone pain score, change in bone turnover markers, and safety. After a median follow up of 11.9 months, the SRE rate was 22% and 23.2% in the ZOMETA® every 4 weeks group and ZOMETA® every 12 weeks group respectively (P=0.724), suggesting that ZOMETA® given every 12 weeks was non-inferior to the q 4 week regimen. The secondary endpoints were comparable as well. More patients had renal toxicities in the ZOMETA® q 4 week group vs q 12 week group (9.6% vs 7.9%, respectively) and two cases (1.0%) of OsteoNecrosis of the Jaw (ONJ) were reported in the ZOMETA® q 4 week group. The authors concluded that the efficacy of continuing ZOMETA® for an additional year at the q 12 week schedule was non-inferior to ZOMETA® given q 4 weeks, among patients who had initially received IV bisphosphonates monthly, for one year or longer. Further the less frequent dosing of ZOMETA® compared with the standard monthly dosing, may be more convenient for the patients and result in less toxicities. Hortobagyi GN, Lipton A, Chew HK, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA9500)
Category: Meeting Updates
Efficacy and safety of the anti-PD-1 monoclonal antibody MK-3475 in 411 patients (pts) with melanoma (MEL)
SUMMARY: It is estimated that in the US, approximately 76,000 new cases of melanoma will be diagnosed and close to 8000 individuals will die of the disease in 2014. The incidence of melanoma has been on the rise for the past three decades. Unlike other malignancies, the role of chemotherapy for the treatment of melanoma has been limited. Treatment of advanced melanoma with immunotherapy using a cytokine, Interleukin-2 (IL-2) produced by T cells during an immune response, was first explored in the mid 1970’s. Durable responses were noted in a very small percentage of patients but this was associated with significant toxicities. This however opened the doors for the development of various immunotherapies, with a better understanding of the Immune checkpoints. Immune checkpoints are cell surface inhibitory proteins/receptors that harness the immune system and prevent uncontrolled immune reactions. Survival of cancer cells in the human body may be to a significant extent, related to their ability to escape immune surveillance, by inhibiting T lymphocyte activation. The T cells of the immune system play a very important role in modulating the immune system. Under normal circumstances, inhibition of an intense immune response, by switching off the T cells of the immune system, is an evolutionary mechanism and is accomplished by Immune checkpoints or Gate Keepers. With the recognition of Immune checkpoint proteins and their role in suppressing antitumor immunity, antibodies are being developed that target the membrane bound inhibitory Immune checkpoint proteins/receptors such as CTLA-4 (Cytotoxic T-Lymphocyte Antigen 4, also known as CD152), PD-1 (Programmed cell Death-1), etc. By doing so, one would expect to unleash the T cells, resulting in T cell proliferation, activation and a therapeutic response. The first immune checkpoint protein to be clinically targeted was CTLA-4. YERVOY® (Ipilimumab), an antibody that blocks Immune checkpoint protein/receptor CTLA- 4, has been shown to prolong overall survival in patients with previously treated, unresectable or metastatic melanoma.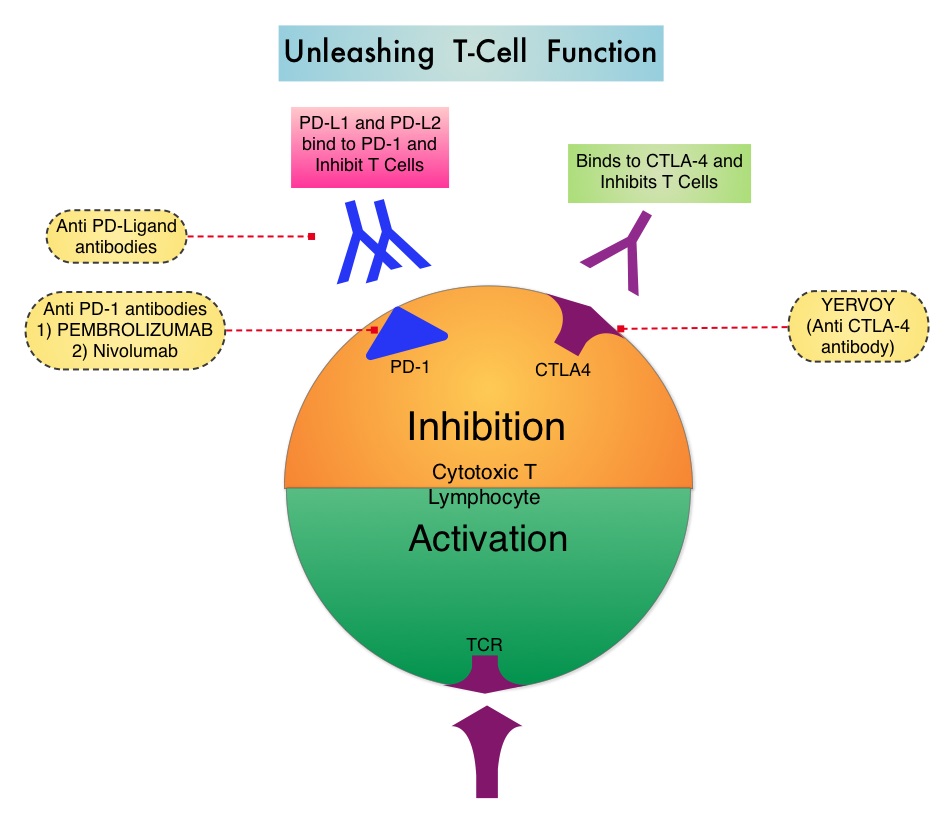 The Food and Drug Administration in May 2014, granted Pembrolizumab a Priority Review designation under its Accelerated Approval Program. Pembrolizumab was previously granted a Breakthrough Therapy designation for advanced melanoma. The authors in this largest phase I clinical trial ever done in patients with malignant melanoma, evaluated the efficacy and safety of Pembrolizumab (formerly known as MK-3475, Lambrolizumab), a humanized monoclonal IgG4 anti PD-1 antibody, in a pooled analysis of 411 patients with advanced melanoma. Of these patients, 221 patients had prior therapy with Ipilimumab (YERVOY® ) and 190 patients were YERVOY® naïve. In this study, three different dosing schedules for Pembrolizumab were utilized – 2 mg/kg every three weeks (N=162), 10 mg/kg every three weeks (N=192) and 10 mg/kg every two weeks (N=57). At the time of this analysis, all patients had at least 6 months of follow up and 75% of the patients had been followed up for at least 9 months. The Overall Response Rate was 40% in the YERVOY® naïve group and 28% in the YERVOY® treated group. Responses were durable and ongoing (88% ongoing) at the time of this analysis. The duration of responses ranged from 6 to 76 weeks, and the median response duration has not yet been reached. The median Progression Free Survival was 24 weeks in YERVOY® naïve group and 23 weeks in the YERVOY® treated group. The median Overall Survival has not been reached at the time of this analysis and the estimated 1 year Overall Survival rate for all patients was 71%. The activity with Pembrolizumab was demonstrated across all dose levels and patient subgroups, irrespective of prior YERVOY® therapy, performance status, LDH levels, BRAF mutation status, tumor stage, and number, as well as type of prior therapies. The most common adverse events of any grade were fatigue, pruritus and rash. Only 4% of the patients discontinued treatment due to a drug related toxicities and overall, 12% of patients experienced grade 3/4 adverse events. The authors concluded that the PD-1 targeting antibody, Pembrolizumab, produced durable responses in patients with advanced melanoma, regardless of prior therapy with YERVOY® and this benefit was accomplished with minimal toxicities. This efficacy data is comparable to another PD-1 targeted monoclonal antibody, Nivolumab. Because of the lack of cross resistance between anti PD-1 antibodies and YERVOY®, combining PD-1 targeted monoclonal antibody with a CTLA-4 targeted antibody such as YERVOY®, could potentially be synergistic, with better outcomes. Ribas A, Hodi FS, Kefford R, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA 9000)</s
The Food and Drug Administration in May 2014, granted Pembrolizumab a Priority Review designation under its Accelerated Approval Program. Pembrolizumab was previously granted a Breakthrough Therapy designation for advanced melanoma. The authors in this largest phase I clinical trial ever done in patients with malignant melanoma, evaluated the efficacy and safety of Pembrolizumab (formerly known as MK-3475, Lambrolizumab), a humanized monoclonal IgG4 anti PD-1 antibody, in a pooled analysis of 411 patients with advanced melanoma. Of these patients, 221 patients had prior therapy with Ipilimumab (YERVOY® ) and 190 patients were YERVOY® naïve. In this study, three different dosing schedules for Pembrolizumab were utilized – 2 mg/kg every three weeks (N=162), 10 mg/kg every three weeks (N=192) and 10 mg/kg every two weeks (N=57). At the time of this analysis, all patients had at least 6 months of follow up and 75% of the patients had been followed up for at least 9 months. The Overall Response Rate was 40% in the YERVOY® naïve group and 28% in the YERVOY® treated group. Responses were durable and ongoing (88% ongoing) at the time of this analysis. The duration of responses ranged from 6 to 76 weeks, and the median response duration has not yet been reached. The median Progression Free Survival was 24 weeks in YERVOY® naïve group and 23 weeks in the YERVOY® treated group. The median Overall Survival has not been reached at the time of this analysis and the estimated 1 year Overall Survival rate for all patients was 71%. The activity with Pembrolizumab was demonstrated across all dose levels and patient subgroups, irrespective of prior YERVOY® therapy, performance status, LDH levels, BRAF mutation status, tumor stage, and number, as well as type of prior therapies. The most common adverse events of any grade were fatigue, pruritus and rash. Only 4% of the patients discontinued treatment due to a drug related toxicities and overall, 12% of patients experienced grade 3/4 adverse events. The authors concluded that the PD-1 targeting antibody, Pembrolizumab, produced durable responses in patients with advanced melanoma, regardless of prior therapy with YERVOY® and this benefit was accomplished with minimal toxicities. This efficacy data is comparable to another PD-1 targeted monoclonal antibody, Nivolumab. Because of the lack of cross resistance between anti PD-1 antibodies and YERVOY®, combining PD-1 targeted monoclonal antibody with a CTLA-4 targeted antibody such as YERVOY®, could potentially be synergistic, with better outcomes. Ribas A, Hodi FS, Kefford R, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA 9000)</s
Randomized comparison of ibrutinib versus ofatumumab in relapsed or refractory (R/R) chronic lymphocytic leukemia/small lymphocytic lymphoma Results from the phase III RESONATE trial
SUMMARY: The American Cancer Society estimates that approximately 15,720 new cases of chronic lymphocytic leukemia (CLL) will be diagnosed in 2014 and approximately 4600 patients will die from the disease. CLL is a disease of the elderly and the average age at the time of diagnosis is 72 years. There are two main types of lymphocytes, B and T lymphocytes/cells, and B-cell CLL is the most common type of leukemia in adults. Normal B-cell activation and proliferation is dependent on B-cell receptor (BCR) signaling.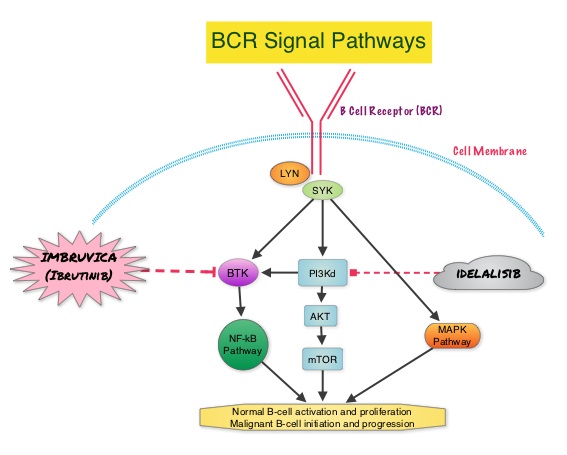 This signaling is also important for initiation and progression of B-cell lymphoproliferative disorders. Bruton’s tyrosine kinase (BTK) is a member of the Tec family of kinases, downstream of the B-cell receptor and is predominantly expressed in B-cells. It is a mediator of B-cell receptor signaling in normal and transformed B-cells. Following binding of antigen to the BCR, Syk (Spleen Tyrosine Kinase), Lyn (member of the Src family of protein tyrosine kinases) and BTK (Bruton’s Tyrosine Kinase) are activated, with subsequent propagation through PI3K/Akt, MAPK, and NF-κB pathways and resulting B-cell activation and proliferation. IMBRUVICA® (Ibrutinib) is an oral, irreversible inhibitor of BTK and inhibits cell proliferation and promotes programmed cell death (Apoptosis). The RESONATE trial is a multicenter, randomized, open-label Phase III study in which single agent IMBRUVICA® was compared to single agent ARZERRA® (Ofatumumab) in patients with relapsed or refractory CLL or Small Lymphocytic Lymphoma (SLL). In this study, 391 patients who had measurable nodal disease and received at least one prior therapy, were randomized to receive 420 mg of IMBRUVICA® orally once daily until progression (N=195) or ARZERRA® at an initial dose of 300 mg followed by 11 doses at 2000 mg, given intravenously weekly (N=196). Patients randomized to the ARZERRA® group, on disease progression were allowed to receive treatment with IMBRUVICA®. The median age was 67 years, 40% of the patients enrolled in the study were 70 years of age or over and 30% of patients had deletion of chromosome 17p. The primary endpoint of this study was Progression-Free Survival (PFS) and the secondary endpoints included Overall Survival (OS), Overall Response rate (ORR) and safety. Following recommendations from the Independent Data Monitoring Committee (IDMC), the study was stopped earlier, as the primary endpoint as well as an important secondary endpoint of the study, were met. At a median follow up of 9.4 months, IMBRUVICA® significantly prolonged PFS compared to ARZERRA® (median not reached vs 8.1 months; HR 0.215, P<0.0001) with a 78.5% reduction in the risk of disease progression and also significantly improved OS (median not reached, HR 0.43, P=0.0049) when compared with ARZERRA®, with a 57% reduction in the risk of death. The Overall Response Rates were significantly higher in the IMBRUVICA® group compared to the ARZERRA® group (42.6% vs 4.1% (P <0 .0001). An additional 20% of patients treated with IMBRUVICA® had a partial response of their persistent lymphocytosis. The benefit with IMBRUVICA® was similarly high even in the two very high risk groups of patients such as those with 17p deletions and those refractory to purine analog chemoimmunotherapy. The overall survival was significant despite the crossover of 57 patients upon progression, from the ARZERRA® group to IMBRUVICA®. Treatment was well tolerated in both groups. Diarrhea, fatigue, nausea and atrial fibrillation were more frequent in the IMBRUVICA® group but did not result in frequent dose reductions or treatment discontinuation. The authors concluded that IMBRUVICA® significantly improved Progression Free Survival, Overall Survival and Overall Response Rates, in patients with relapsed/refractory CLL/SLL, compared with ARZERRA® and IMBRUVICA® should also be a consideration for elderly patients who often are unable to tolerate intensive chemotherapy. Byrd JC, Brown JR, O’Brien SM, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA7008)
This signaling is also important for initiation and progression of B-cell lymphoproliferative disorders. Bruton’s tyrosine kinase (BTK) is a member of the Tec family of kinases, downstream of the B-cell receptor and is predominantly expressed in B-cells. It is a mediator of B-cell receptor signaling in normal and transformed B-cells. Following binding of antigen to the BCR, Syk (Spleen Tyrosine Kinase), Lyn (member of the Src family of protein tyrosine kinases) and BTK (Bruton’s Tyrosine Kinase) are activated, with subsequent propagation through PI3K/Akt, MAPK, and NF-κB pathways and resulting B-cell activation and proliferation. IMBRUVICA® (Ibrutinib) is an oral, irreversible inhibitor of BTK and inhibits cell proliferation and promotes programmed cell death (Apoptosis). The RESONATE trial is a multicenter, randomized, open-label Phase III study in which single agent IMBRUVICA® was compared to single agent ARZERRA® (Ofatumumab) in patients with relapsed or refractory CLL or Small Lymphocytic Lymphoma (SLL). In this study, 391 patients who had measurable nodal disease and received at least one prior therapy, were randomized to receive 420 mg of IMBRUVICA® orally once daily until progression (N=195) or ARZERRA® at an initial dose of 300 mg followed by 11 doses at 2000 mg, given intravenously weekly (N=196). Patients randomized to the ARZERRA® group, on disease progression were allowed to receive treatment with IMBRUVICA®. The median age was 67 years, 40% of the patients enrolled in the study were 70 years of age or over and 30% of patients had deletion of chromosome 17p. The primary endpoint of this study was Progression-Free Survival (PFS) and the secondary endpoints included Overall Survival (OS), Overall Response rate (ORR) and safety. Following recommendations from the Independent Data Monitoring Committee (IDMC), the study was stopped earlier, as the primary endpoint as well as an important secondary endpoint of the study, were met. At a median follow up of 9.4 months, IMBRUVICA® significantly prolonged PFS compared to ARZERRA® (median not reached vs 8.1 months; HR 0.215, P<0.0001) with a 78.5% reduction in the risk of disease progression and also significantly improved OS (median not reached, HR 0.43, P=0.0049) when compared with ARZERRA®, with a 57% reduction in the risk of death. The Overall Response Rates were significantly higher in the IMBRUVICA® group compared to the ARZERRA® group (42.6% vs 4.1% (P <0 .0001). An additional 20% of patients treated with IMBRUVICA® had a partial response of their persistent lymphocytosis. The benefit with IMBRUVICA® was similarly high even in the two very high risk groups of patients such as those with 17p deletions and those refractory to purine analog chemoimmunotherapy. The overall survival was significant despite the crossover of 57 patients upon progression, from the ARZERRA® group to IMBRUVICA®. Treatment was well tolerated in both groups. Diarrhea, fatigue, nausea and atrial fibrillation were more frequent in the IMBRUVICA® group but did not result in frequent dose reductions or treatment discontinuation. The authors concluded that IMBRUVICA® significantly improved Progression Free Survival, Overall Survival and Overall Response Rates, in patients with relapsed/refractory CLL/SLL, compared with ARZERRA® and IMBRUVICA® should also be a consideration for elderly patients who often are unable to tolerate intensive chemotherapy. Byrd JC, Brown JR, O’Brien SM, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA7008)
CALGB/SWOG 80405 Phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with KRAS wild-type (wt) untreated metastatic adenocarcinoma of the colon or rectum (MCRC)
SUMMARY: The American Cancer Society estimates that approximately 137,000 new cases of colorectal cancer will be diagnosed in the United States in 2014 and over 50,000 are expected to die of the disease. Even though colon cancer localized to the bowel is potentially curable with surgery and adjuvant chemotherapy, advanced colon cancer is often incurable. Standard chemotherapy when combined with anti EGFR (Epidermal Growth Factor Receptor) targeted monoclonal antibodies such as VECTIBIX® (Panitumumab) and ERBITUX® (Cetuximab) as well as anti VEGF agent AVASTIN® (Bevacizumab), have demonstrated improvement in Progression Free Survival and Overall Survival.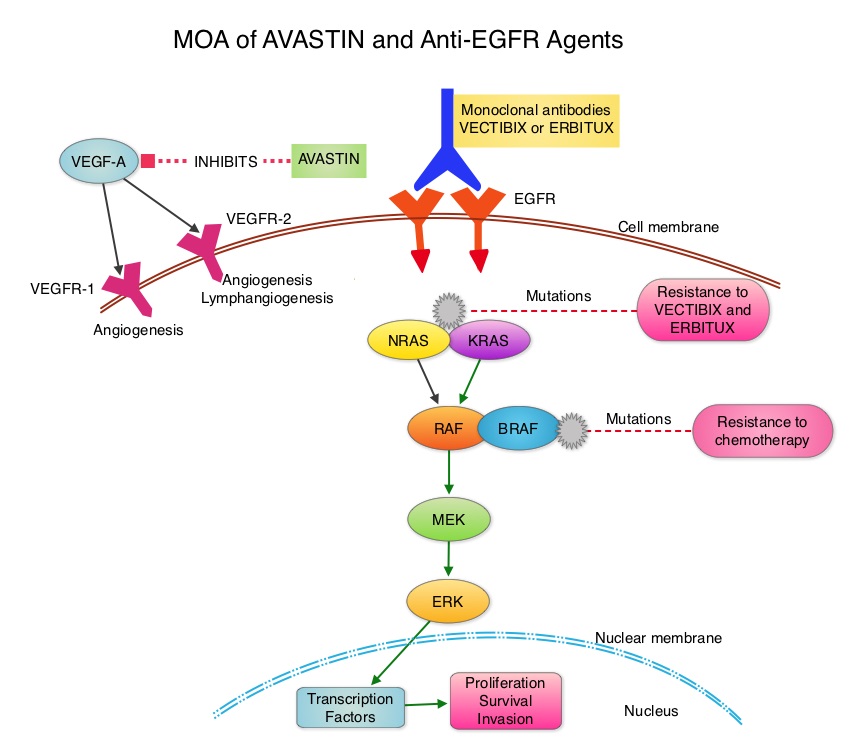 The benefit with anti EGFR agents however is only demonstrable in patients with metastatic colon cancer, whose tumors do not harbor KRAS mutations in codons 12 and 13 of exon 2 (KRAS Wild Type). It is now becoming clear that even amongst the KRAS Wild Type patient groups, about 15% to 20% have other rare mutations such as NRAS and BRAF mutations, which confer resistance to anti EGFR agents. Therefore, pan RAS (expanded RAS) testing may become relevant. To determine the optimal combination treatment regimen, this phase III intergroup trial evaluated the addition of ERBITUX® or AVASTIN® to physician’s choice of standard first line chemotherapy such as FOLFIRI or mFOLFOX6. Even though the original study included unselected metastatic colorectal cancer patients and randomization to a third arm (combination of ERBITUX® and AVASTIN®), this study was amended to include only pts with KRAS Wild Type tumors and the combination ERBITUX® and AVASTIN® arm was deleted. Patients were randomized to either ERBITUX® 400 mg/m2 week one and then 250 mg/m2, weekly or AVASTIN® 5 mg/kg every 2 weeks given along with FOLFIRI or mFOLFOX6 chemotherapy (physicians choice at the time of enrollment). The median age was 59 years and treatment groups were Chemo plus AVASTIN® (N=559) and Chemo plus ERBITUX® (N=578). Approximately 27% of the patients received FOLFIRI chemotherapy regimen and 76% received mFOLFOX6 chemotherapy regimen. Treatment was given until disease progression and median follow up was 24 months. The primary endpoint was Overall Survival. The median Overall Survival was similar in the ERBITUX® combination and the AVASTIN® combination groups (about 29 months) and so was the Progression Free Survival in both groups (about 10.5 months). The chemotherapy used with either of the antibodies had no influence on the outcomes. The toxicity profiles were different as expected, with increased incidence of Grade 3-4 rash (7% versus 0%) and diarrhea (11% versus 8%), in the ERBITUX® group and increased incidence of Grade 3-4 hypertension (7% versus 1%) and gastrointestinal events (2% versus 0.5%), in the AVASTIN® group. The authors concluded that either ERBITUX® or AVASTIN® in combination with chemotherapy have equivalent overall survival benefit, when given as first line therapy, for patients with metastatic colorectal cancer, whose tumors are KRAS Wild Type. It remains to be seen however, if pan RAS (expanded RAS) testing and other molecular studies will identify subsets of patients who will benefit from specific antibody chemotherapy combination regimens. Venook AP, Niedzwiecki D, Lenz H, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA3)
The benefit with anti EGFR agents however is only demonstrable in patients with metastatic colon cancer, whose tumors do not harbor KRAS mutations in codons 12 and 13 of exon 2 (KRAS Wild Type). It is now becoming clear that even amongst the KRAS Wild Type patient groups, about 15% to 20% have other rare mutations such as NRAS and BRAF mutations, which confer resistance to anti EGFR agents. Therefore, pan RAS (expanded RAS) testing may become relevant. To determine the optimal combination treatment regimen, this phase III intergroup trial evaluated the addition of ERBITUX® or AVASTIN® to physician’s choice of standard first line chemotherapy such as FOLFIRI or mFOLFOX6. Even though the original study included unselected metastatic colorectal cancer patients and randomization to a third arm (combination of ERBITUX® and AVASTIN®), this study was amended to include only pts with KRAS Wild Type tumors and the combination ERBITUX® and AVASTIN® arm was deleted. Patients were randomized to either ERBITUX® 400 mg/m2 week one and then 250 mg/m2, weekly or AVASTIN® 5 mg/kg every 2 weeks given along with FOLFIRI or mFOLFOX6 chemotherapy (physicians choice at the time of enrollment). The median age was 59 years and treatment groups were Chemo plus AVASTIN® (N=559) and Chemo plus ERBITUX® (N=578). Approximately 27% of the patients received FOLFIRI chemotherapy regimen and 76% received mFOLFOX6 chemotherapy regimen. Treatment was given until disease progression and median follow up was 24 months. The primary endpoint was Overall Survival. The median Overall Survival was similar in the ERBITUX® combination and the AVASTIN® combination groups (about 29 months) and so was the Progression Free Survival in both groups (about 10.5 months). The chemotherapy used with either of the antibodies had no influence on the outcomes. The toxicity profiles were different as expected, with increased incidence of Grade 3-4 rash (7% versus 0%) and diarrhea (11% versus 8%), in the ERBITUX® group and increased incidence of Grade 3-4 hypertension (7% versus 1%) and gastrointestinal events (2% versus 0.5%), in the AVASTIN® group. The authors concluded that either ERBITUX® or AVASTIN® in combination with chemotherapy have equivalent overall survival benefit, when given as first line therapy, for patients with metastatic colorectal cancer, whose tumors are KRAS Wild Type. It remains to be seen however, if pan RAS (expanded RAS) testing and other molecular studies will identify subsets of patients who will benefit from specific antibody chemotherapy combination regimens. Venook AP, Niedzwiecki D, Lenz H, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA3)
Randomized comparison of adjuvant aromatase inhibitor (AI) exemestane (E) plus ovarian function suppression (OFS) vs tamoxifen (T) plus OFS in premenopausal women with hormone receptor-positive (HR+) early breast cancer (BC) Joint analysis of IBCSG TEXT and SOFT trials
SUMMARY: Breast cancer is the most common cancer among women in the US and about 1 in 8 women (12%) will develop invasive breast cancer during their lifetime. Approximately, 233,000 new cases of invasive breast cancer will be diagnosed in 2014 and 40,000 women will die of the disease. Approximately 75% of patients with breast cancer are hormone receptor positive (Estrogen Receptor/Progesterone Receptor positive) and this is a predictor of response to endocrine therapy. In premenopausal woman, the ovary is the main source of estrogen production, whereas in postmenopausal women, the primary source of estrogen is the Aromatase enzyme mediated conversion of androstenedione and testosterone to estrone and estradiol in extragonadal/peripheral tissues.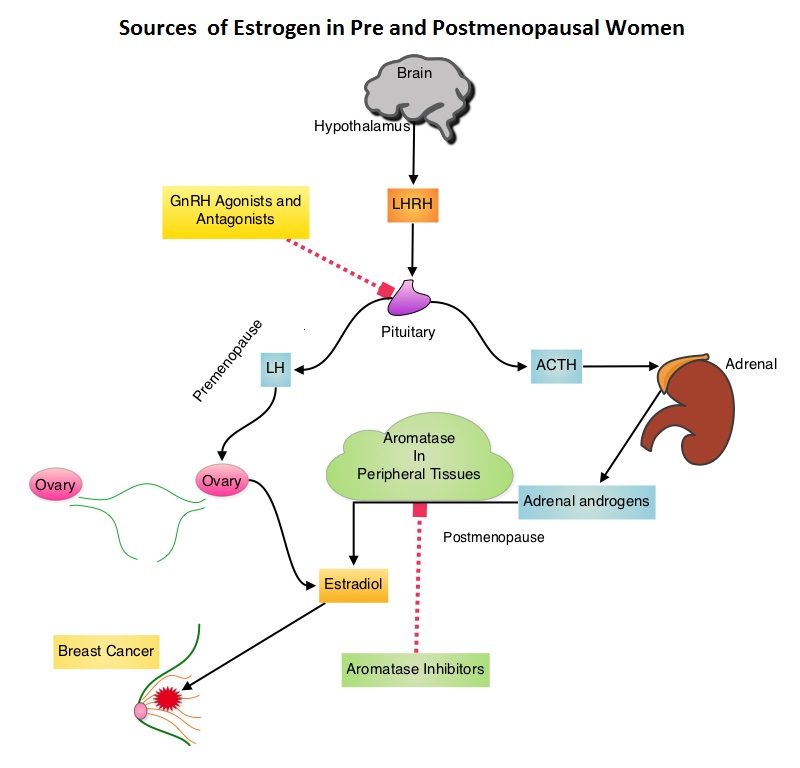 Presently available therapies include Tamoxifen and other Selective ER Modulators, which modulate ER alpha activity, Aromatase Inhibitors and Ovarian ablation that decrease estrogen production and FASLODEX® (Fulvestrant) that down regulates Estrogen Receptor. Aromatase Inhibitors (AI’s) are often prescribed, due to their superiority over Tamoxifen, for postmenopausal women with Hormone Receptor positive breast tumors, in adjuvant as well as metastatic settings. AI’s however, are not effective in premenopausal women, as these individuals derive their estrogen mainly from ovaries and not extragonadal tissues. The 2000 Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) overview, as well as subsequent studies comparing adjuvant ovarian ablation/suppression with adjuvant chemotherapy in premenopausal women with hormone positive breast tumors, have demonstrated similar magnitude of benefit. The TEXT (Tamoxifen and Exemestane Trial) and SOFT (Suppression of Ovarian Function Trial) are two phase III randomized trials, conducted at the same time and included premenopausal women (average age was 43 years) with hormone receptor positive early breast cancer. In the joint analysis of these two trials in which 5738 women were enrolled, the authors set out to answer 2 important questions – whether adjuvant AI improves outcomes in this patient group when their Ovarian Function is suppressed and whether there is any benefit with Ovarian Function suppression in premenopausal women suitable for adjuvant Tamoxifen. TEXT randomized patients (N=2672) within 3 months of surgery to 5 years of AROMASIN® (Exemestane) plus Ovarian Function Suppression (OFS) or 5 years of Tamoxifen plus OFS. The SOFT study randomized patients (N=3066) to 5 years of AROMASIN® plus OFS or 5 years of Tamoxifen plus OFS or 5 years of Tamoxifen alone. OFS choices included oophorectomy, ovarian irradiation or 5 years of TRELSTAR® (Triptorelin), a GnRH (Gonadotropin Releasing Hormone) agonist. The primary endpoint of these two studies was Disease Free Survival (DFS). In this joint analysis the outcomes for 4690 women randomized to receive AROMASIN® plus OFS or Tamoxifen plus OFS for 5 years, were analyzed. The 5 year Disease Free Survival was 91.1% in the AROMASIN® plus OFS group and 87.3% in the Tamoxifen plus OFS group (HR=0.72, P<0.0002). Compared to patients receiving Tamoxifen plus OFS, AROMASIN® plus OFS reduced the relative risk of premenopausal women developing a subsequent invasive breast cancer by 28% and the relative risk of breast cancer recurrence by 34%. The authors concluded that this largest joint analysis, evaluating adjuvant AI therapy with OFS in premenopausal women with Hormone receptor positive breast cancer, has demonstrated that 5 years of highly effective adjuvant endocrine therapy without chemotherapy can result in excellent outcomes. Further, AROMASIN® may be better than tamoxifen, when given with Ovarian Function Suppression. Pagani O, Regan MM, Walley B, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA1)
Presently available therapies include Tamoxifen and other Selective ER Modulators, which modulate ER alpha activity, Aromatase Inhibitors and Ovarian ablation that decrease estrogen production and FASLODEX® (Fulvestrant) that down regulates Estrogen Receptor. Aromatase Inhibitors (AI’s) are often prescribed, due to their superiority over Tamoxifen, for postmenopausal women with Hormone Receptor positive breast tumors, in adjuvant as well as metastatic settings. AI’s however, are not effective in premenopausal women, as these individuals derive their estrogen mainly from ovaries and not extragonadal tissues. The 2000 Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) overview, as well as subsequent studies comparing adjuvant ovarian ablation/suppression with adjuvant chemotherapy in premenopausal women with hormone positive breast tumors, have demonstrated similar magnitude of benefit. The TEXT (Tamoxifen and Exemestane Trial) and SOFT (Suppression of Ovarian Function Trial) are two phase III randomized trials, conducted at the same time and included premenopausal women (average age was 43 years) with hormone receptor positive early breast cancer. In the joint analysis of these two trials in which 5738 women were enrolled, the authors set out to answer 2 important questions – whether adjuvant AI improves outcomes in this patient group when their Ovarian Function is suppressed and whether there is any benefit with Ovarian Function suppression in premenopausal women suitable for adjuvant Tamoxifen. TEXT randomized patients (N=2672) within 3 months of surgery to 5 years of AROMASIN® (Exemestane) plus Ovarian Function Suppression (OFS) or 5 years of Tamoxifen plus OFS. The SOFT study randomized patients (N=3066) to 5 years of AROMASIN® plus OFS or 5 years of Tamoxifen plus OFS or 5 years of Tamoxifen alone. OFS choices included oophorectomy, ovarian irradiation or 5 years of TRELSTAR® (Triptorelin), a GnRH (Gonadotropin Releasing Hormone) agonist. The primary endpoint of these two studies was Disease Free Survival (DFS). In this joint analysis the outcomes for 4690 women randomized to receive AROMASIN® plus OFS or Tamoxifen plus OFS for 5 years, were analyzed. The 5 year Disease Free Survival was 91.1% in the AROMASIN® plus OFS group and 87.3% in the Tamoxifen plus OFS group (HR=0.72, P<0.0002). Compared to patients receiving Tamoxifen plus OFS, AROMASIN® plus OFS reduced the relative risk of premenopausal women developing a subsequent invasive breast cancer by 28% and the relative risk of breast cancer recurrence by 34%. The authors concluded that this largest joint analysis, evaluating adjuvant AI therapy with OFS in premenopausal women with Hormone receptor positive breast cancer, has demonstrated that 5 years of highly effective adjuvant endocrine therapy without chemotherapy can result in excellent outcomes. Further, AROMASIN® may be better than tamoxifen, when given with Ovarian Function Suppression. Pagani O, Regan MM, Walley B, et al. J Clin Oncol 32:5s, 2014 (suppl; abstr LBA1)
Placebo controlled, double blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors (PROMID) Results on long-term survival
SUMMARY: The role of Somatostatin analogs such as SANDOSTATIN® (Octreotide) for symptom control in patients with gastrointestinal and pancreatic NeuroEndocrine Tumors (NETs) is well established. SANDOSTATIN® also demonstrated antiproliferative activity in controlling tumor growth of well-differentiated metastatic midgut NETs (Carcinoid), by lengthening the Time to Tumor Progression (TTP), when compared with placebo (PROMID Study). Whether SANDOSTATIN® prolongs Overall Survival (OS) remained unclear. The study investigators now reported the long term follow up data from the same PROMID trial. Between 2001 and 2008, 85 patients were randomly assigned to receive either SANDOSTATIN® LAR (N=42) or Placebo (N=43). On disease progression, patients in the placebo group were allowed to crossover and receive SANDOSTATIN® LAR. Outcomes in patients with Hepatic tumor Load (HL – percentage of liver replaced by malignancy) at study entry of 10% or less, was compared to those whose HL was more than 10%. The median OS by January 2013 in the Placebo arm was 84 months whereas the median OS in the SANDOSTATIN® LAR group was not reached, suggesting that the OS in this group will exceed 84 months and therefore a longer follow up would be needed. Patients with HL 10% or less benefited the most whereas those with high HL did not have OS benefit with SANDOSTATIN® LAR. The authors concluded that SANDOSTATIN® LAR prolongs TTP as well as OS in patients with metastatic midgut NETs, carrying a Hepatic Load of 10% or less. Arnold R, Wittenberg M, Rinke A, et al. J Clin Oncol 31, 2013 (suppl; abstr 4030)
A Phase 3, Randomized, Double-Blind, Placebo-Controlled Study Evaluating the Efficacy and Safety of Idelalisib and Rituximab for Previously Treated Patients with Chronic Lymphocytic Leukemia (CLL)
SUMMARY: PI3K delta signaling is hyperactive in B-cell malignancies and is important for the activation, proliferation, homing of malignant B cells in the lymphoid tissues and their survival. The delta isoform of PI3K enzyme is predominantly expressed in leukocytes. Idelalisib is a highly selective oral inhibitor of the enzyme phosphoinositide 3-kinase (PI3K) and specifically blocks the delta isoform of PI3K enzyme and its signaling pathway. Following promising data from Phase I trials, a Phase III study was conducted in which 220 previously treated patients with recurrent CLL, measurable lymphadenopathy and ineligible to receive chemotherapy due to comorbidities, were enrolled. Patients received first dose of RITUXAN® (Rituximab) at 375 mg/m2 and then 500 mg/m2 q2 weeks x 4, followed by RITUXAN® q4 wks x 3 for a total of 8 doses along with Idelalisib 150 mg PO BID continuously until disease progression (N=110) or along with placebo. The median age was 71 years and patients had received a median of three prior therapies. Poor prognosis patients included 44% with 17p deletion/p53 mutation and 84% who had unmutated immunoglobulin variable region heavy chain (IgVH) gene. Primary endpoint was progression-free survival (PFS). Following a recommendation by an Independent Data Monitoring Committee after an interim analysis that showed superiority of RITUXAN®/Idelalisib combination, this trial was stopped early. The PFS at 24 weeks was 93% for the RITUXAN® plus Idelalisib group compared to 46% for those treated with RITUXAN® and placebo. The median PFS for the RITUXAN®/Idelalisib combination group has not yet been reached, whereas the the median PFS for the RITUXAN®/placebo arm was 5.5 months (Hazard Ratio [HR] = 0.15; P < .0001). Further, the PFS was favorable in the poor prognosis patients with either a 17p deletion or p53 mutation, when Idelalisib was combined with RITUXAN® (HR = 0.12). An improvement in the Overall Survival (OS) was also noted in the Idelalisib group compared with patients in the RITUXAN® alone group (HR = 0.28; P = 0.018). The combination of Idelalisib and RITUXAN® had an overall response rate of 81% compared with 13% in the RITUXAN®alone group (P <0 .0001). Patients treated with a combination of Idelalisib and RITUXAN® also had a higher decrease in lymphadenopathy (93%) compared with 4% in the RITUXAN® alone group (P < 0.0001). The most common adverse events which included pyrexia, fatigue, nausea and chills were similar in both treatment groups. The authors concluded that Idelalisib plus RITUXAN® may be a new treatment option for patients with previously treated CLL, who are not eligible for chemotherapy, as well as those with unfavorable cytogenetics. Furman RR, Sharman JP, Coutre SE, et al. Blood 2013;122:LBA-6
PROSE: Randomized proteomic stratified phase III study of second line erlotinib versus chemotherapy in patients with inoperable non–small cell lung cancer (NSCLC)
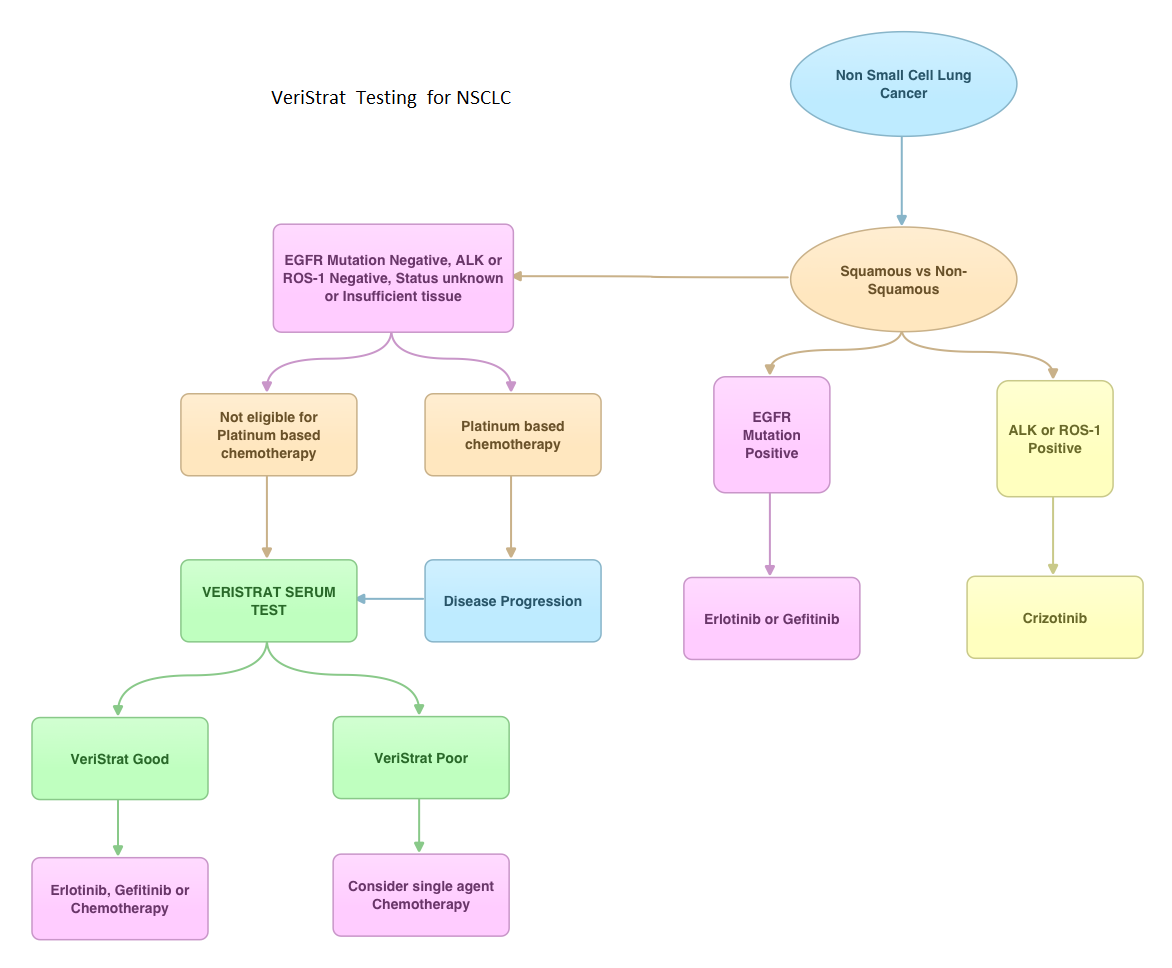
SUMMARY: VeriStrat ® is a clinically validated serum/plasma-based assay, for patients with advanced Non Small Cell Lung Cancer (NSCLC). VeriStrat® is a serum test of prognostic and predictive value that classifies patients as VeriStrat-Good (VS-G) or VeriStrat-Poor (VS-P) based on eight mass spectral peaks or proteomic patterns of the patients serum. Proteomics is the large-scale study of protein structure and functions. VeriStrat® testing is protein based and therefore has no correlation with known genomic biomarkers. It is well established that EGFR-TKIs (Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitors) are more effective in NSCLC patients with EGFR activating mutations. PROSE is a multicenter, double blind, randomized, VeriStrat® stratified, phase III study. In this trial, over 90% of the patients had no EGFR mutations (EGFR-Wild Type). Two hundred and eighty five (285) patients with advanced NSCLC who had first line treatment regimen with platinum-based therapy were randomly assigned to receive second line chemotherapy (CT) with single agent ALIMTA® (Pemetrexed) or TAXOTERE® (Docetaxel), at standard doses (N=129) or TARCEVA® (Erlotinib) 150 mg po qd (N=134). Patients and study investigators were blinded to the patients VeriStrat® status. Patients were classified as VeriStrat-Good or VeriStrat-Poor based on the VeriStrat® results. Patients in the treatment groups were stratified by age, gender, tumor histology, ECOG-PS and smoking history. Crossover was permitted upon disease progression. The primary objective of the study was to demonstrate differential treatment benefit between TARCEVA® and CT with regards to Overall Survival (OS). Median overall survival (OS) was 9 months for the patients in the CT group and 7.7 months for TARCEVA® group and this was not statistically significant (P=0.3). However when evaluated by VeriStrat® status, CT was beneficial for the VeriStrat-Poor patients compared to TARCEVA®, with significantly better median OS (6.3 vs 3 months, P=0.02). Age, gender, histology (squamous vs non-squamous) and smoking history had no impact on the overall survival. The authors concluded that patients classified as VeriStrat-Poor have better survival with CT than TARCEVA®, whereas patients classified as VeriStrat-Good have similar survival with TARCEVA® and CT. VeriStrat® testing therefore, can help physicians choose between TARCEVA® and CT, for their patients with advanced NSCLC. This test helps physicians identify patients who are likely to have good or poor outcomes after treatment with EGFR inhibitors and thereby can provide valuable insight into whether CT or targeted therapy with TARCEVA®, a EGFR-TKI, is appropriate for their patients with advanced NSCLC, in the second line setting. This information is especially important for patients without an EGFR mutation or for those, whose EGFR mutation status is unknown. Sorlini C, Barni S, Petrelli F, et al. J Clin Oncol 29: 2011 (suppl; abstr TPS214)
PROSE Randomized proteomic stratified phase III study of second line erlotinib versus chemotherapy in patients with inoperable non–small cell lung cancer (NSCLC)
SUMMARY: VeriStrat ® is a clinically validated serum/plasma-based assay, for patients with advanced Non Small Cell Lung Cancer (NSCLC). VeriStrat® is a serum test of prognostic and predictive value that classifies patients as VeriStrat-Good (VS-G) or VeriStrat-Poor (VS-P) based on eight mass spectral peaks or proteomic patterns of the patients serum. Proteomics is the large-scale study of protein structure and functions. VeriStrat® testing is protein based and therefore has no correlation with known genomic biomarkers. It is well established that EGFR-TKIs (Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitors) are more effective in NSCLC patients with EGFR activating mutations. PROSE is a multicenter, double blind, randomized, VeriStrat® stratified, phase III study. In this trial, over 90% of the patients had no EGFR mutations (EGFR-Wild Type). Two hundred and eighty five (285) patients with advanced NSCLC who had first line treatment regimen with platinum-based therapy were randomly assigned to receive second line chemotherapy (CT) with single agent ALIMTA® (Pemetrexed) or TAXOTERE® (Docetaxel), at standard doses (N=129) or TARCEVA® (Erlotinib) 150 mg po qd (N=134). Patients and study investigators were blinded to the patients VeriStrat® status. Patients were classified as VeriStrat-Good or VeriStrat-Poor based on the VeriStrat® results. Patients in the treatment groups were stratified by age, gender, tumor histology, ECOG-PS and smoking history. Crossover was permitted upon disease progression. The primary objective of the study was to demonstrate differential treatment benefit between TARCEVA® and CT with regards to Overall Survival (OS). Median overall survival (OS) was 9 months for the patients in the CT group and 7.7 months for TARCEVA® group and this was not statistically significant (P=0.3). However when evaluated by VeriStrat® status, CT was beneficial for the VeriStrat-Poor patients compared to TARCEVA®, with significantly better median OS (6.3 vs 3 months, P=0.02). Age, gender, histology (squamous vs non-squamous) and smoking history had no impact on the overall survival. The authors concluded that patients classified as VeriStrat-Poor have better survival with CT than TARCEVA®, whereas patients classified as VeriStrat-Good have similar survival with TARCEVA® and CT. VeriStrat® testing therefore, can help physicians choose between TARCEVA® and CT, for their patients with advanced NSCLC. This test helps physicians identify patients who are likely to have good or poor outcomes after treatment with EGFR inhibitors and thereby can provide valuable insight into whether CT or targeted therapy with TARCEVA®, a EGFR-TKI, is appropriate for their patients with advanced NSCLC, in the second line setting. This information is especially important for patients without an EGFR mutation or for those, whose EGFR mutation status is unknown. Sorlini C, Barni S, Petrelli F, et al. J Clin Oncol 29: 2011 (suppl; abstr TPS214)
Randomized comparison of FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment of KRAS wild-type metastatic colorectal cancer German AIO study KRK-0306 (FIRE-3)
SUMMARY: It is common practice to combine anti-EGFR agent ERBITUX® (Cetuximab) or anti-VEGF agent AVASTIN® (Bevacizumab) with chemotherapy, in the initial management of patients with metastatic colorectal cancer. There is however a higher likelihood for patients with tumors expressing wild type KRAS (non-mutated KRAS), to respond to ERBITUX®. In this randomized multicenter study, a CAMPTOSAR® (Irinotecan) based backbone, FOLFIRI (folinic acid, fluorouracil and Irinotecan) given along with ERBITUX® (Group A) was compared with FOLFIRI plus AVASTIN® (Group B), in treatment naïve patients with metastatic ColoRectal Cancer (mCRC). Of the 592 patients with wild type KRAS mCRC, 297 patients were randomized to Group A and 295 patients to Group B. The median age was 64 years. The median duration of treatment was 4.7 months and 5.3 months in Group A and Group B respectively. The primary endpoint was Objective Response Rate (ORR). Even though the ORR was comparable in Groups A and B (62% vs 57%), there was a significant improvement in the overall survival (OS) favoring Group A (28.8 vs 25.0 months, HR= 0.77, P=0.0164). The comparable response rates and surprising improvement in OS in the ERBITUX® group suggests that either ERBITUX® or AVASTIN® can be added to FOLFIRI, in the first-line treatment of wild type KRAS mCRC patients. It is however clear that in wild type KRAS mCRC patients, it may be harmful to combine ERBITUX® with FOLFOX chemotherapy regimen, as was seen in the EPOCH trial and based on MRC COIN trial, NORDIC-VII trial and N0147 trial, ERBITUX® should not be combined with FOLFOX chemotherapy regimen as there is no added benefit. It is now well established that mCRC that harbors KRAS mutations in exon 2 (about 40% of the patients) do not benefit from anti-EGFR therapies. The PRIME study has given us aditional insight and it appears that other activating RAS mutations may also predict lack of response to anti-EGFR therapies. With regards to BRAF mutations, they portend a poor prognosis, regardless of treatment. Heinemann V, Weikersthal LF, Decker T, et al. J Clin Oncol 31, 2013 (suppl; abstr LBA3506)
