SUMMARY: Bones are the third most common site of metastatic disease and approximately 100,000 cases of bone metastasis are reported in the United States each year. Cancers originating in the breast, prostate, lung, thyroid and kidney, are more likely to metastasize to the bone. Bisphosphonates inhibit osteoclast-mediated bone resorption and both oral and IV bisphosphonates reduce the risk of developing Skeletal Related Events (SRE’s) and delay the time to SRE’s in patients with bone metastases. Bisphosphonates can also reduce bone pain and may improve Quality of life. Intravenous bisphosphonates, Pamidronate (AREDIA®) and Zoledronic acid (ZOMETA®) have been approved in the US for the treatment of bone metastases. ZOMETA®, a third generation amino-bisphosphonate, has however largely replaced AREDIA® because of its superior efficacy, reducing pain and the incidence of Skeletal Related Events, by 25% to 40%. Both AREDIA® and ZOMETA® are administered IV every 3 to 4 weeks, following diagnoses of bone metastases. However, the optimal treatment schedule has remained unclear. Further, renal toxicity, long bone fractures and OsteoNecrosis of the Jaw (ONJ) have been identified as potential toxicities and the incidence of these toxicities increase with cumulative drug exposure.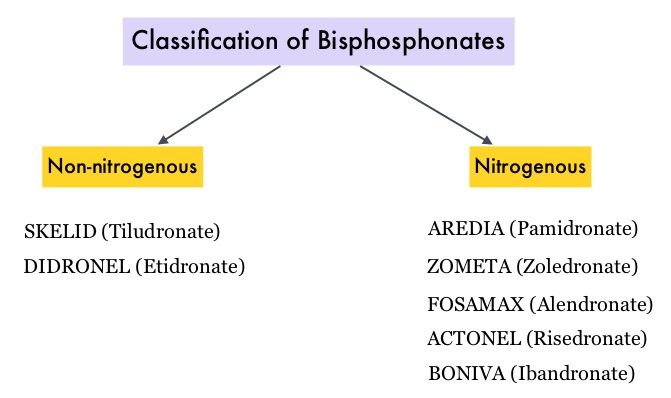
The purpose of this study was to determine whether ZOMETA® administered every 12 weeks was non-inferior to ZOMETA® administered every 4 weeks. In this open-label, non-inferiority trial, 1822 patients were enrolled (Breast,N=855, Prostate,N=689 and Myeloma,N=278), and were randomly assigned in a 1:1 ratio to receive ZOMETA® every 4 weeks or every 12 weeks, for 2 years. The median age was 65 yrs and patients had at least one site of bone involvement. The Primary endpoint was incidence of at least one Skeletal Related Event within 2 years (defined as clinical fracture, spinal cord compression, radiation to bone, or surgery involving bone) after randomization. Secondary endpoints included skeletal morbidity rates (mean number of Skeletal Related Events per year), performance status, pain using the Brief Pain Inventory and incidences of ONJ and renal dysfunction. Both treatment groups were well matched. Patients in this trial were stratified by disease and analyses by disease, was pre-planned.
In the 795 patients who completed the study at 2 years, 29.5% of patients receiving ZOMETA® every 4 weeks and 28.6% of patients receiving ZOMETA® every 12 weeks experienced at least 1 Skeletal Related Event and this was not significantly different. With regards to Secondary endpoints, there were still no significant differences between the two treatment groups with regards to Pain scores, performance status scores, incidence of jaw osteonecrosis, and kidney dysfunction.
The authors concluded that ZOMETA® administered every 3 months for 2 years is non-inferior to ZOMETA®administered every 4 weeks for 2 years, among patients with breast cancer, prostate cancer and multiple myeloma, with bone metastases. A less frequent dosing of ZOMETA® compared with the standard monthly dosing, may also be more convenient for the patients and cost effective. XGEVA®, a RANK ligand (RANKL) inhibitor is also approved in the US for the treatment of bone metastases from solid tumors. A study is underway comparing XGEVA® administered every 4 weeks to every 12 weeks, in patients with metastatic breast and prostate cancer. Effect of Longer-Interval vs Standard Dosing of Zoledronic Acid on Skeletal Events in Patients With Bone Metastases. A Randomized Clinical Trial. Himelstein AL, Foster JC, Khatcheressian JL, et al. JAMA. 2017;317:48-58

