SUMMARY: Patients with Thrombotic Thrombocytopenic Purpura (TTP), Heparin Induced Thrombocytopenia (HIT) and Immune Thrombocytopenic Purpura (ITP) often receive prophylactic platelet transfusions even though there are no data to support this practice. These transfusions are often given preemptively to reduce the risk for spontaneous bleeding in patients who are thrombocytopenic. Thrombocytopenia refers to a platelet count below the lower limit of the normal range used by the laboratory performing the count. In the United States, a little over 2 million platelet units are transfused annually.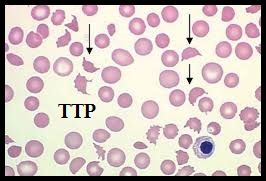 The known risks associated with platelet transfusion include febrile and allergic reactions, Transfusion Related Acute Lung Injury and infections. The authors in this study utilized a Nationwide Inpatient Sample of patients over a 5 year period from 2007-2011and evaluated the risks associated with platelet transfusions.
The known risks associated with platelet transfusion include febrile and allergic reactions, Transfusion Related Acute Lung Injury and infections. The authors in this study utilized a Nationwide Inpatient Sample of patients over a 5 year period from 2007-2011and evaluated the risks associated with platelet transfusions.  They identified 10,624 hospitalizations with TTP and platelet transfusions were reported in 10.1%, 6,332 hospitalizations with HIT and 7.1% received platelet transfusions and 79,980 admissions with ITP and 25.8% received platelet transfusions. The Odds Ratio (OR) was calculated after adjusting for age, gender, clinical severity and acuity. (An Odds Ratio is a measure of association between an exposure and an outcome. The OR represents the odds that an outcome will occur given a particular exposure, compared to the odds of the outcome occurring in the absence of that exposure). The researchers noted some alarming findings. Platelet transfusions in TTP were associated with higher odds of arterial thrombosis (OR=5.8), Acute Myocardial Infarction (OR=2.0) and mortality (OR=2.0). Platelet transfusions in HIT were associated with higher odds of arterial thrombosis (OR=3.4) and mortality (OR=5.2). Platelet transfusions in TTP or HIT however, was not associated with venous thrombosis. There were no increased risks among patients with ITP, who received platelet transfusions. The authors concluded that until future trials provide additional information, platelet transfusions should be considered a relative contraindication in patients with TTP and HIT and should only be used in situations where severe or potentially life threatening bleeding is refractory to other therapies. Platelet transfusions in platelet consumptive disorders are associated with arterial thrombosis and in-hospital mortality. Goel R, Ness PM, Takemoto CM, et al. Blood. 2015;125:1470-1476.
They identified 10,624 hospitalizations with TTP and platelet transfusions were reported in 10.1%, 6,332 hospitalizations with HIT and 7.1% received platelet transfusions and 79,980 admissions with ITP and 25.8% received platelet transfusions. The Odds Ratio (OR) was calculated after adjusting for age, gender, clinical severity and acuity. (An Odds Ratio is a measure of association between an exposure and an outcome. The OR represents the odds that an outcome will occur given a particular exposure, compared to the odds of the outcome occurring in the absence of that exposure). The researchers noted some alarming findings. Platelet transfusions in TTP were associated with higher odds of arterial thrombosis (OR=5.8), Acute Myocardial Infarction (OR=2.0) and mortality (OR=2.0). Platelet transfusions in HIT were associated with higher odds of arterial thrombosis (OR=3.4) and mortality (OR=5.2). Platelet transfusions in TTP or HIT however, was not associated with venous thrombosis. There were no increased risks among patients with ITP, who received platelet transfusions. The authors concluded that until future trials provide additional information, platelet transfusions should be considered a relative contraindication in patients with TTP and HIT and should only be used in situations where severe or potentially life threatening bleeding is refractory to other therapies. Platelet transfusions in platelet consumptive disorders are associated with arterial thrombosis and in-hospital mortality. Goel R, Ness PM, Takemoto CM, et al. Blood. 2015;125:1470-1476.

