SUMMARY: The FDA granted breakthrough therapy designation to Nivolumab (OPDIVO®), as a treatment for patients with recurrent or metastatic Squamous Cell Carcinoma of the Head and Neck (SCCHN), following a platinum based therapy. This designation was based on the findings from CheckMate-141 study, which demonstrated an improvement in Overall Survival (OS) with OPDIVO®, compared to investigator’s choice of therapy. The American Cancer Society estimates that 61,760 people will be diagnosed with Head and Neck cancer in 2016 and 13,190 patients will die of the disease. Patients with recurrent/metastatic Squamous Cell Carcinoma of the Head and Neck (SCCHN) have a poor prognosis with a median Overall Survival (OS) of about 13 months with first line therapy and about 6 months or less with later lines of therapy. The treatment paradigm for solid tumors has been rapidly evolving with a better understanding of the Immune checkpoints or gate keepers. Immune checkpoints are cell surface inhibitory proteins/receptors that are expressed on activated T cells. They harness the immune system and prevent uncontrolled immune reactions. Survival of cancer cells in the human body may be to a significant extent related to their ability to escape immune surveillance by inhibiting T lymphocyte activation. The T cells of the immune system therefore play a very important role in modulating the immune system. Under normal circumstances, inhibition of an intense immune response and switching off the T cells of the immune system, is an evolutionary mechanism and is accomplished by Immune checkpoints or gate keepers. With the recognition of Immune checkpoint proteins and their role in suppressing antitumor immunity, antibodies are being developed that target the membrane bound inhibitory Immune checkpoint proteins/receptors such as CTLA-4 (Cytotoxic T-Lymphocyte Antigen 4, also known as CD152), PD-1(Programmed cell Death 1), etc. By doing so, one would expect to unleash the T cells, resulting in T cell proliferation, activation and a therapeutic response.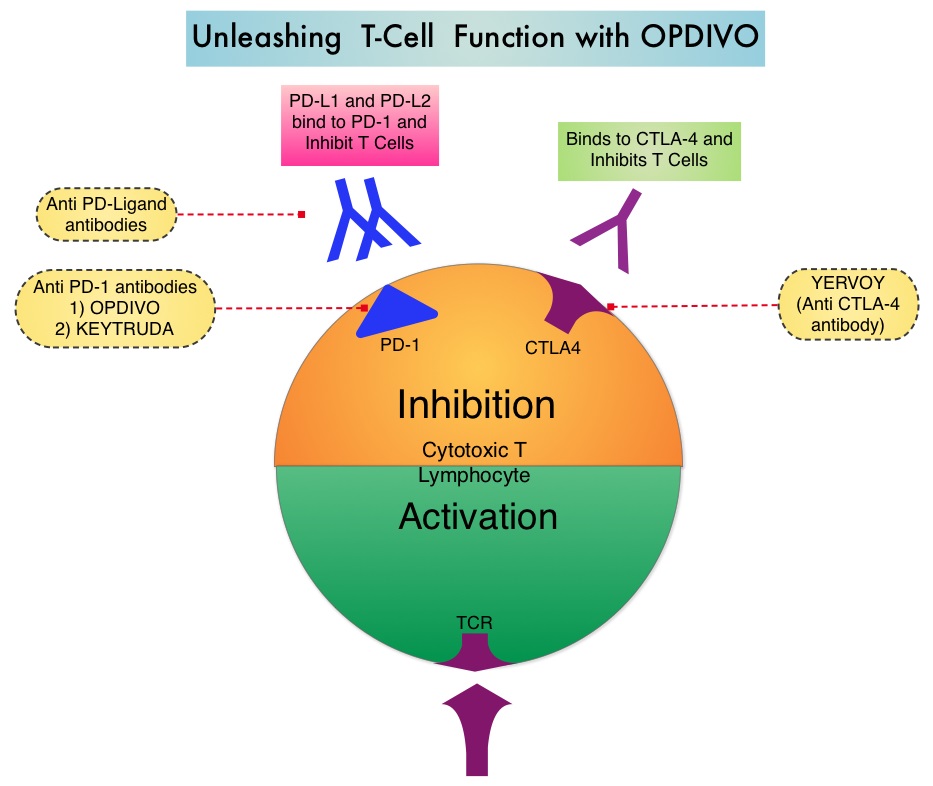
OPDIVO® is a fully human, immunoglobulin G4 monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, thereby undoing PD-1 pathway-mediated inhibition of the immune response. CheckMate-141 is an open-label, phase III trial, in which 361 patients with recurrent or metastatic Squamous Cell Carcinoma of the oral cavity, pharynx, or larynx, were randomly assigned in a 2:1 ratio to receive either OPDIVO® (N= 240) or investigator’s choice of ERBITUX® (Cetuximab), TAXOTERE® (Docetaxel) or Methotrexate (N=121). OPDIVO® was administered intravenously at 3 mg/kg every 2 weeks. ERBITUX® dosing was 400 mg/m2 for the first dose followed by 250 mg/m2 weekly, TAXOTERE® dosing was 30 mg/m2 weekly and Methotrexate dosing was 40 mg/m2 weekly. The median age was 60 years, majority of patients were male, had received 2 or more prior systemic therapies and prior radiation therapy. Patients were stratified based on prior therapy with monoclonal antibody, ERBITUX® and HPV status was known for 50% of the participants. The primary endpoint was Overall Survival and secondary endpoints included Response Rates and Progression Free Survival (PFS).
This study was stopped earlier than scheduled after an independent monitoring panel determined that the primary endpoint for this study was met, with significant superiority of OPDIVO® over the investigator’s choice of therapy. The median Overall Survival with OPDIVO® was 7.5 months, compared to 5.1 months with investigator’s choice of therapy (HR=0.70; P=0.010). The 1-year Overall Survival with OPDIVO® was 36%, which was more than double, compared with investigator’s choice of therapy, which was 16.6%. Patients with PD-L1 expression of 1% or more benefited the most from treatment with OPDIVO®, with a median OS of 8.7 months, compared to 4.6 months in the control group (HR=0.55). For patients with PD-L1 expression less than 1%, median OS was 5.7 with OPDIVO® versus 5.8 months, for the control group (HR=0.89). HPV status also had an impact on outcomes. HPV-positive patients had a median OS of 9.1 months with OPDIVO® compared with 4.4 months with investigator’s choice of therapy (HR=0.56), whereas those who were HPV-negative and receiving OPDIVO®, had a median OS of 7.5 months compared to 5.8 months with investigator’s choice of therapy (HR=0.73). Grade 3 or 4 adverse events were significantly lower with OPDIVO®, compared with investigator’s choice of therapy(13.1% vs 35.1%).
The authors concluded that OPDIVO® is the first agent to demonstrate a significant improvement in Overall Survival, in patients with advanced head and neck cancer following progression on platinum-based chemotherapy, and fulfills an unmet need for this patient group. Gillison ML, Blumenschein G, Fayette J, et al. Nivolumab Versus Investigator’s Choice (IC) for Recurrent or Metastatic (R/M) Head and Neck Squamous Cell Carcinoma (SCCHN): CheckMate-141. Presented at: AACR 2016 Annual Meeting, New Orleans; April 16-20, 2016. Abstract CT099.

