SUMMARY: Prostate Cancer is the most common cancer in American men with the exclusion of skin cancer, and 1 in 9 men will be diagnosed with Prostate Cancer during their lifetime. It is estimated that in the United States, about 191,930 new cases of Prostate Cancer will be diagnosed in 2020 and 33,330 men will die of the disease. The five year survival among patients first diagnosed with metastatic disease is approximately 30%. Early detection and treatment may improve outcomes. Risk factors for Prostate Cancer include age, ethnicity, and family history of Prostate Cancer. In individuals with a family history of Prostate Cancer in one or more first-degree relatives, the Relative Risk of Prostate Cancer increases approximately 2-3 fold, and the risk increases with an increasing number of affected relatives, and is inversely related to the age at time of diagnosis among those relatives.
It is estimated that approximately 40% of all diagnosed Prostate Cancers are inherited and Prostate Cancer risk also has been implicated in other familial cancer syndromes such as Hereditary Breast and Ovarian Cancer (HBOC) syndrome and Lynch Syndrome (LS). HBOC syndrome typically is found in families with early onset cancer and multiple cancer diagnoses such as, breast, ovarian and pancreatic cancer. Tumor suppressor DNA repair genes BRCA1 and BRCA2, has been implicated in Prostate Cancer, particularly in HBOC families. Patients with a BRCA1 mutation have a nearly 2-fold Relative Risk of Prostate Cancer among men less than 65 years, whereas those with BRCA2 mutations have a more than 7 fold Relative Risk. Further, patients with BRCA2 mutations are also associated with clinically aggressive disease, progression, and higher rates of cancer-specific mortality. It is estimated that the frequency of BRCA2 mutations ranges from 1-3%. The National Comprehensive Cancer Network (NCCN) recommends that BRCA2 mutation carriers begin Prostate Cancer screening with PSA testing and a digital rectal exam by age 40, and that BRCA1 mutation carriers consider testing at age 40, as well.
Lynch Syndrome, or Hereditary Non-Polyposis Colorectal Cancer, is associated with germline DNA mismatch repair defects, and individuals with Lynch Syndrome are 2-5 times more likely to develop Prostate Cancer during their lifetimes.
The purpose of this population-based study was to quantify the Relative Risk of Prostate Cancer associated with different family cancer histories such as Hereditary Prostate Cancer, Hereditary Breast and Ovarian Cancer syndrome and Lynch Syndrome. The Utah Population Database was chosen as it is very large and linked to the Utah Cancer Registry. The Relative Risk for Prostate Cancer in general, as well as the risks for three Prostate Cancer subgroups- early onset, lethal, and clinically significant Prostate Cancers, was evaluated.
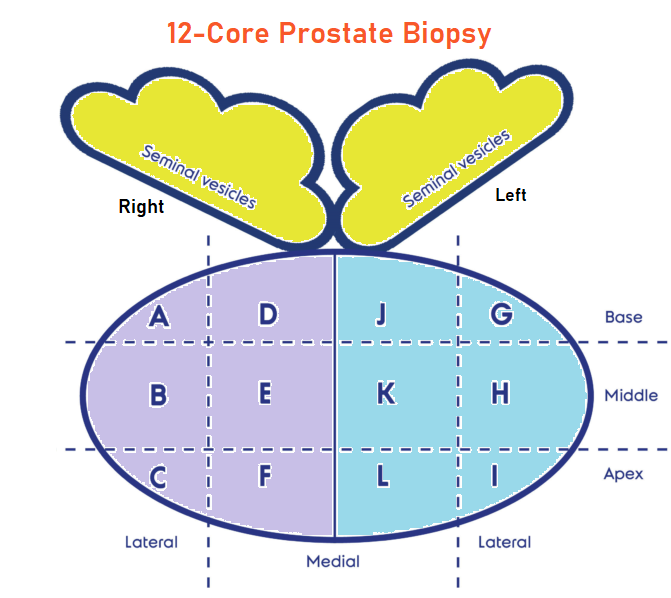
The authors using the Utah Population Database identified 619,630 men, 40 years or older, who were members of a pedigree that included at least 3 consecutive generations. Each individual was then assessed for family history of Hereditary Prostate Cancer, Hereditary Breast and Ovarian Cancer (HBOC) or Lynch syndrome, as well as his own Prostate Cancer status. The participant’s own cancer disease status was not used in any of the family history definitions. Family history of Hereditary Prostate Cancer was defined as 3 or more first-degree relatives with Prostate Cancer, or Prostate Cancer in 3 or more affected relatives diagnosed in 3 successive generations of the same lineage (paternal or maternal), or 2 or more first-degree relatives both diagnosed with early-onset disease (55 years or less). The NCCN Guidelines for BRCA-related Breast and/or Ovarian Cancer Syndrome were adapted for a family history of HBOC and revised Bethesda Guidelines were adapted for Lynch Syndrome, to determine if an individual had a positive family history of Lynch Syndrome. All Prostate Cancer occurences were classified into one or more subtypes: Early-onset Prostate Cancer defined as Prostate Cancer diagnosed at age 55 years or less, Lethal Prostate Cancer was identified if Prostate Cancer was listed as the primary cause of death on a death certificate, and Clinically significant Prostate Cancer if the Gleason score was 7 or more, direct extension, regional lymph node involvement or presence of distant metastases.
The overall prevalence of Prostate Cancer for the cohort was 5.9% (N=36,360), of whom 7% had Early onset disease, 11.1% had Lethal disease and 41.8% had Clinically significant disease. The median age at time of diagnosis was 69 years, approximately 70% of men were diagnosed with organ-confined disease, and approximately 6% were first diagnosed with metastatic disease.
Family history of Hereditary Prostate Cancer was associated with the highest risk for all Prostate Cancer subtypes combined, with a 2.3-fold increase in risk for Prostate Cancer overall (Relative Risk 2.30). This was followed by Hereditary Breast and Ovarian Cancer, with a Relative Risk of 1.47, and Lynch syndrome with a Relative Risk of 1.16.
Hereditary Prostate Cancer was associated with a near 4-fold increase in risk for early onset Prostate Cancer (RR=3.93). Hereditary Prostate Cancer also was associated with higher risks for both Lethal Prostate Cancer (RR=2.21) and Clinically significant disease (RR=2.32). Overall, modest elevations in risk were associated with Lynch Syndrome, with a 34% increase in risk for early onset disease (RR=1.34) and a small increase in the risk for Clinically significant disease (RR=1.15).
It was concluded from this investigation of a large, population-based family database that, targeting high-risk populations such as those with Hereditary Prostate Cancer early, with genetic screening and cancer surveillance, is indicated. This study also demonstrated the importance of well-ascertained family history information, for determining Prostate Cancer risk, as well as determining important Prostate Cancer subsets such as Early onset and Lethal disease. The authors added that this is the first study that compared the risk of Prostate Cancer in men with Hereditary Prostate Cancer, with families having HBOC or Lynch syndrome in the same population.
Risk of Prostate Cancer Associated With Familial and Hereditary Cancer Syndromes. Beebe-Dimmer JL, Kapron AL, Fraser AM, et al. J Clin Oncol. 2020;38:1807-1813