SUMMARY: Prostate cancer is the most common cancer in American men with the exclusion of skin cancer, and 1 in 9 men will be diagnosed with prostate cancer during their lifetime. It is estimated that in the United States, about 191,930 new cases of prostate cancer will be diagnosed in 2020 and 33,330 men will die of the disease. TransRectal UltraSound (TRUS) guided biopsy has been the standard of care for diagnosing prostate cancer in men with a clinical suspicion of prostate cancer, based on an abnormal Digital Rectal Examination and/or an elevated Prostate Specific Antigen (PSA) level. TransRectal UltraSound (TRUS) guided biopsy is a blind biopsy of the lateral and posterior peripheral zone of the prostate using a template, and 10 to 12 cores of prostate tissue is obtained (Systematic Biopsy). Even though this may result in a higher rate of prostate cancer detection, many detected cancers are low grade tumors that do not benefit from treatment, and these patients are on active surveillance for their low risk disease. The major limitation of this biopsy procedure is the risk of under-sampling a more significant tumor that is located in a region of the prostate not usually targeted with a template. Further, in patients with a rising PSA with a prior negative biopsy, patients are often subjected to a repeat blind biopsy with the same limitations as the original biopsy. Since biopsy access is through the rectum and only specific zones of the prostate are sampled, large areas of the prostate, especially the anterior and central prostate, are not routinely sampled and clinically significant higher-grade cancers are sometimes missed.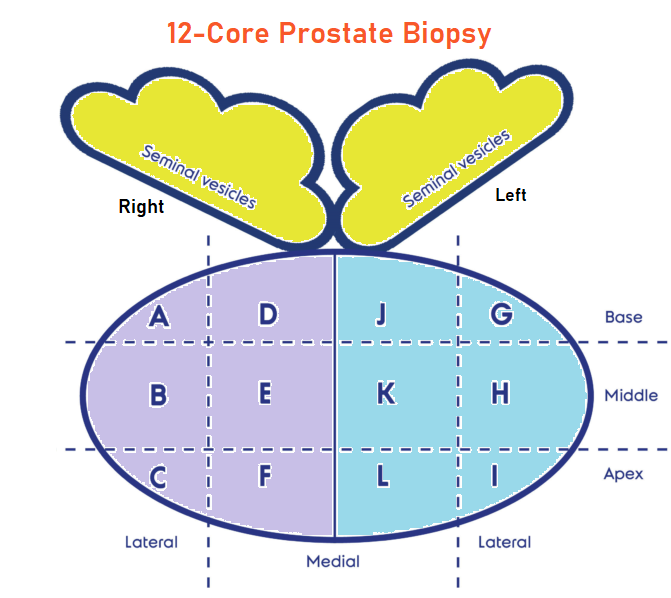
Multiparametric MRI (mp-MRI) combines anatomic imaging in the form of T2-weighted imaging, with functional imaging and is being used to detect or rule out cancer in men who have persistent concern for prostate cancer. Previously published studies have shown that MRI-targeted biopsies alone have shown similar or higher rates of detection of clinically SIGNIFICANT cancer in the prostate gland (high grade cancers) and lower rates of detection of clinically INSIGNIFICANT cancer, when compared to systematic biopsy (standard TRUS guided biopsy). This interesting advantage appears to allow the use of mp-MRI as a triage test to avoid a biopsy if the results were negative, and if positive could be used for targeting abnormal areas in the prostate during biopsy. Despite this advantage, debate persists whether MRI-targeted biopsy should be used in place of systematic biopsy or in conjunction with it.
The Trio Study is a substudy of a larger clinical trial called, Use of Tracking Devices to Locate Abnormalities During Invasive Procedures. In this substudy, the authors assessed the use of MRI-targeted, systematic, or combined MRI-targeted and systematic prostate biopsy, in an attempt to define the most effective method for prostate cancer diagnosis.
In this study a total of 2732 men with abnormal PSA or Digital Rectal Exam underwent prostate MRI. Among these patients, 2103 men had MRI-visible lesions and subsequently underwent both MRI-targeted and systematic biopsies. Grade group 1 refers to clinically INSIGNIFICANT disease (Gleason score, 3+3=6), Grade group 2 or higher refers to cancer with favorable intermediate risk or worse (Gleason score, 3+4=7), and Grade group 3 or higher refers to clinically SIGNIFICANT cancer with unfavorable intermediate risk or worse (Gleason score, 4+3=7). The Primary outcome of this study was cancer detection rates according to Grade group (Clustering of Gleason grades) for each biopsy method, and in combination.
Among all 2103 patients who underwent the two biopsy methods, prostate cancer was diagnosed in 52.5% with systematic biopsy alone and in 51.5% with MRI-targeted biopsy alone. The addition of MRI-targeted biopsy to systematic biopsy led to 208 more prostate cancer diagnoses for a total prostate cancer diagnosis of 62.4%. MRI-targeted biopsy detected more clinically SIGNIFICANT Grade group 3 or higher cancers than systematic biopsy (P=0.004) and detected fewer cancers in Grade group 1 (P<0.001). Of the 404 patients who subsequently underwent radical prostatectomy, disease upgrading on histopathology occurred in 41.6% of patients when compared to findings on systematic biopsy alone, 30.9% when compared with findings on MRI-targeted biopsy alone and 14.4% when compared with findings on combined systematic and MRI-targeted biopsy.
The authors concluded that among patients with MRI-visible lesions, a combination of systematic and MRI-targeted biopsy increases the detection of clinically significant prostate cancers, compared to either strategy alone. MRI-Targeted, Systematic, and Combined Biopsy for Prostate Cancer Diagnosis. Ahdoot M, Wilbur AR, Reese SE, et al. N Engl J Med 2020; 382:917-928

