SUMMARY: It is estimated that approximately 20% of cancer patients in the US take Omega-3 fatty acids in the form of fish oil. Fish oil is a mixture of fatty acids produced from several species of fish and the two most abundant and important fatty acids in fish oil include EicosaPentaenoic Acid (EPA) and DocosaHexaenoic Acid (DHA). Fish oil content in presently available preparations is not standardized and does not require FDA approval. Preclinical studies have demonstrated that mouse tumors recruit mesenchymal stem cells that are specifically activated by platinum based chemotherapy and secrete 2 fatty acids, 12S-HHT and 16:4(n-3)). These fatty acids are called Platinum Induced Fatty Acids (PIFAs) and they have been shown to induce resistance to a broad range of chemotherapeutic agents, by activating a cytoprotective response in the tumor tissue. 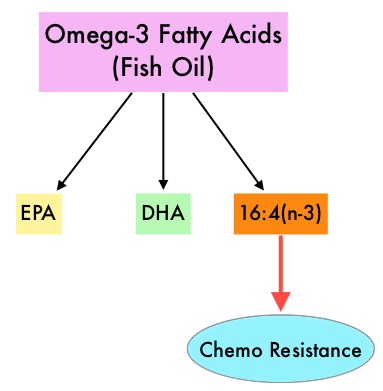 Fish oil has relevant levels of fatty acid 16:4(n-3) and preclinical models have shown that the fish oil neutralized the antitumor activity of chemotherapy, thus conferring drug resistance. With this preclinical information and given that cancer patients frequently use fish oil supplements, the authors evaluated the effect of fish oil intake in healthy volunteers, on the plasma levels of fatty acid 16:4(n-3), which has been shown to induce resistance to chemotherapeutic agents. The researchers first conducted a survey to determine what percentage of cancer patients undergoing treatment at a University Medical Center in the Netherlands were taking fish oil supplements. They also analyzed fatty acid 16:4(n-3) content, in 3 brands of fish oil supplements and 4 often consumed species of fish. The authors then randomly selected 30 healthy volunteers for the fish oil study and 20 healthy volunteers for the fish consumption study and the plasma levels of fatty acid 16:4(n-3) was measured after they consumed fish oil or fish, for a period of 2 weeks. They noted that 11% of the cancer patients in their study reported using omega-3 supplements. All fish oils tested contained amounts of fatty acid 16:4(n-3) ranging from 0.2 to 5.7 μM and this was adequate to induce chemoresistance to a variety of chemotherapeutic agents. They noted that there was a significant rise in the plasma 16:4(n-3) fatty acid levels in the healthy volunteers after they consumed fish oil supplements and fish, with high levels of fatty acid 16:4(n-3). Herring and Mackerel fish contained high levels of fatty acid 16:4(n-3), in contrast to Salmon and Tuna. The authors concluded that based on this preclinical data it is best to avoid fish oils and fish such as Herring and Mackerel in the 48 hours surrounding chemotherapy, as the high plasma 16:4(n-3) fatty acid levels may negate the effects of chemotherapy. These recommendations have been adopted by the Dutch Cancer Society and by the Dutch National Working Group for Oncologic Dieticians. Increased Plasma Levels of Chemoresistance-Inducing Fatty Acid 16:4(n-3) After Consumption of Fish and Fish Oil. Daenen LGM, Cirkel GA, Houthuijzen JM, et al. JAMA Oncol. 2015;1:350-358
Fish oil has relevant levels of fatty acid 16:4(n-3) and preclinical models have shown that the fish oil neutralized the antitumor activity of chemotherapy, thus conferring drug resistance. With this preclinical information and given that cancer patients frequently use fish oil supplements, the authors evaluated the effect of fish oil intake in healthy volunteers, on the plasma levels of fatty acid 16:4(n-3), which has been shown to induce resistance to chemotherapeutic agents. The researchers first conducted a survey to determine what percentage of cancer patients undergoing treatment at a University Medical Center in the Netherlands were taking fish oil supplements. They also analyzed fatty acid 16:4(n-3) content, in 3 brands of fish oil supplements and 4 often consumed species of fish. The authors then randomly selected 30 healthy volunteers for the fish oil study and 20 healthy volunteers for the fish consumption study and the plasma levels of fatty acid 16:4(n-3) was measured after they consumed fish oil or fish, for a period of 2 weeks. They noted that 11% of the cancer patients in their study reported using omega-3 supplements. All fish oils tested contained amounts of fatty acid 16:4(n-3) ranging from 0.2 to 5.7 μM and this was adequate to induce chemoresistance to a variety of chemotherapeutic agents. They noted that there was a significant rise in the plasma 16:4(n-3) fatty acid levels in the healthy volunteers after they consumed fish oil supplements and fish, with high levels of fatty acid 16:4(n-3). Herring and Mackerel fish contained high levels of fatty acid 16:4(n-3), in contrast to Salmon and Tuna. The authors concluded that based on this preclinical data it is best to avoid fish oils and fish such as Herring and Mackerel in the 48 hours surrounding chemotherapy, as the high plasma 16:4(n-3) fatty acid levels may negate the effects of chemotherapy. These recommendations have been adopted by the Dutch Cancer Society and by the Dutch National Working Group for Oncologic Dieticians. Increased Plasma Levels of Chemoresistance-Inducing Fatty Acid 16:4(n-3) After Consumption of Fish and Fish Oil. Daenen LGM, Cirkel GA, Houthuijzen JM, et al. JAMA Oncol. 2015;1:350-358
Category: Hem/Onc Updates
Radiation Therapy Added to Androgen Deprivation Therapy Improves Overall Survival in Locally Advanced Prostate Cancer
SUMMARY:Prostate cancer is the most common cancer in American men with the exclusion of skin cancer and 1 in 7 men will be diagnosed with prostate cancer during their lifetime. It is estimated that in the United States, about 220,800 new cases of prostate cancer will be diagnosed in 2015 and over 27,000 men will die of the disease. The development and progression of prostate cancer is driven by androgens. Androgen Deprivation Therapy (ADT) has therefore been the cornerstone of treatment of advanced prostate cancer and is the first treatment intervention for hormone sensitive prostate cancer. 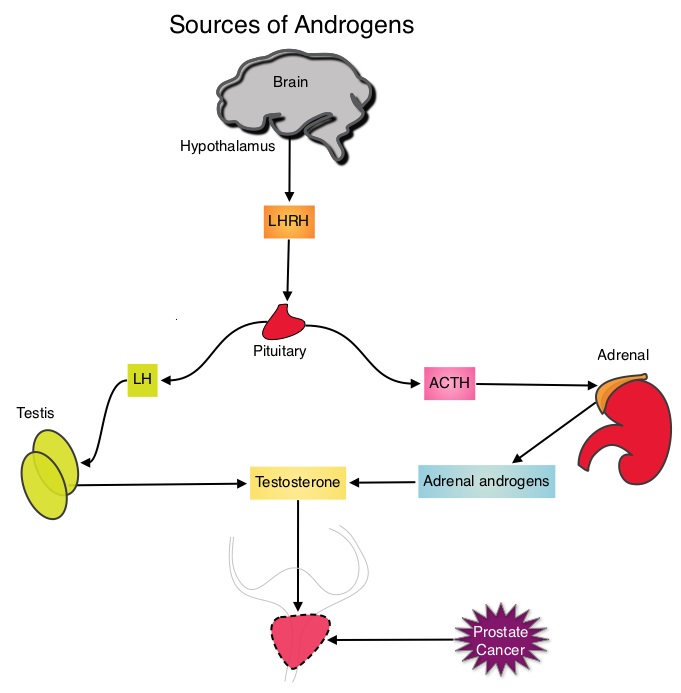 This is accomplished by either surgical castration (bilateral orchiectomy) or medical castration using LHRH (GnRH- Gonadotropin-Releasing Hormone) agonists given along with 2 weeks of first generation anti-androgen agents such as EULEXIN® (Flutamide), CASODEX® (Bicalutamide) or NILANDRON® (Nilutamide), with the anti-androgen agents given to prevent testosterone flare. This large intergroup trial which was developed by the NCIC Clinical Trials Group in collaboration with the Medical Research Council and the National Cancer Institute US Cancer Therapy Evaluation Program, evaluated the benefits of adding Radiation Therapy (RT) to ADT, when compared to ADT alone, in patients with locally advanced prostate cancer. In this study, 1205 patients were randomly assigned to receive either ADT alone (N=602) or ADT plus RT (N=603). Eligible patients included those with T1-2 disease with either Prostate Specific Antigen (PSA) of more than 40 μg/L or PSA of 20-40 μg/L plus Gleason score of 8-10 or patients with T3-4, N0/NX, M0 prostate cancer. ADT consisted of either bilateral orchiectomy or LHRH agonists (plus 2 weeks of oral anti-androgen therapy to prevent testosterone flare), based on patient and physician preference, and ADT was continued for life. RT consisted of a dose of 64-69 Gy given in 35-39 fractions to the prostate gland and pelvis or prostate gland alone. The median age was 70 years and the median follow up was 8 years. Eighty seven percent of patients had T3-4 disease, 63% of patients had a PSA more than 20 μg/L and 18% had a Gleason score of more than 8. The Primary Endpoint was Overall Survival (OS), defined as the time from randomization to death from any cause. Secondary Endpoints included Time To Progression (TTP), improvement in Disease Specific Survival, quality of life and toxicity. The authors had previously reported the interim analysis findings of this intergroup trial and they noted that the addition of RT to ADT significantly improved overall survival, at a median follow up of 6 years (HR= 0.77; P=0.033). In this final analysis, at a median follow up of 8 years, the interim analysis findings were confirmed and the patients assigned to ADT plus RT had significantly improved Overall Survival compared to those who received ADT alone (HR=0.70; P<0.001), with a 30% reduction in the risk of death. Disease Specific Survival was also superior with ADT plus RT compared to ADT alone, with a 54% reduction in deaths from prostate cancer (HR=0.46; P <0 .001). There was a higher incidence of grade 1 and 2 bowel toxicities in patients who received ADT plus RT, but grade 3 bowel toxicities were rare and short term. The authors concluded that this long term follow up data suggests that the addition of Radiation Therapy to Androgen Deprivation Therapy significantly prolongs Overall and Disease Specific Survival, in patients with locally advanced prostate cancer. Final Report of the Intergroup Randomized Study of Combined Androgen-Deprivation Therapy Plus Radiotherapy Versus Androgen-Deprivation Therapy Alone in Locally Advanced Prostate Cancer. Mason MD, Parulekar WR, Sydes MR, et al. J Clin Oncol 2015; 33:2143-2150
This is accomplished by either surgical castration (bilateral orchiectomy) or medical castration using LHRH (GnRH- Gonadotropin-Releasing Hormone) agonists given along with 2 weeks of first generation anti-androgen agents such as EULEXIN® (Flutamide), CASODEX® (Bicalutamide) or NILANDRON® (Nilutamide), with the anti-androgen agents given to prevent testosterone flare. This large intergroup trial which was developed by the NCIC Clinical Trials Group in collaboration with the Medical Research Council and the National Cancer Institute US Cancer Therapy Evaluation Program, evaluated the benefits of adding Radiation Therapy (RT) to ADT, when compared to ADT alone, in patients with locally advanced prostate cancer. In this study, 1205 patients were randomly assigned to receive either ADT alone (N=602) or ADT plus RT (N=603). Eligible patients included those with T1-2 disease with either Prostate Specific Antigen (PSA) of more than 40 μg/L or PSA of 20-40 μg/L plus Gleason score of 8-10 or patients with T3-4, N0/NX, M0 prostate cancer. ADT consisted of either bilateral orchiectomy or LHRH agonists (plus 2 weeks of oral anti-androgen therapy to prevent testosterone flare), based on patient and physician preference, and ADT was continued for life. RT consisted of a dose of 64-69 Gy given in 35-39 fractions to the prostate gland and pelvis or prostate gland alone. The median age was 70 years and the median follow up was 8 years. Eighty seven percent of patients had T3-4 disease, 63% of patients had a PSA more than 20 μg/L and 18% had a Gleason score of more than 8. The Primary Endpoint was Overall Survival (OS), defined as the time from randomization to death from any cause. Secondary Endpoints included Time To Progression (TTP), improvement in Disease Specific Survival, quality of life and toxicity. The authors had previously reported the interim analysis findings of this intergroup trial and they noted that the addition of RT to ADT significantly improved overall survival, at a median follow up of 6 years (HR= 0.77; P=0.033). In this final analysis, at a median follow up of 8 years, the interim analysis findings were confirmed and the patients assigned to ADT plus RT had significantly improved Overall Survival compared to those who received ADT alone (HR=0.70; P<0.001), with a 30% reduction in the risk of death. Disease Specific Survival was also superior with ADT plus RT compared to ADT alone, with a 54% reduction in deaths from prostate cancer (HR=0.46; P <0 .001). There was a higher incidence of grade 1 and 2 bowel toxicities in patients who received ADT plus RT, but grade 3 bowel toxicities were rare and short term. The authors concluded that this long term follow up data suggests that the addition of Radiation Therapy to Androgen Deprivation Therapy significantly prolongs Overall and Disease Specific Survival, in patients with locally advanced prostate cancer. Final Report of the Intergroup Randomized Study of Combined Androgen-Deprivation Therapy Plus Radiotherapy Versus Androgen-Deprivation Therapy Alone in Locally Advanced Prostate Cancer. Mason MD, Parulekar WR, Sydes MR, et al. J Clin Oncol 2015; 33:2143-2150
Tumor genomics May Predict Outcomes with First Line Therapy in Metastatic Renal Cell Carcinoma
SUMMARY: The American Cancer Society estimates that about 61,560 new cases of kidney cancer will be diagnosed in the United States in 2015 and over 14,000 patients will die from this disease. The VHL (Von Hippel-Lindau) gene is the most frequently mutated gene (approximately 90%) in clear cell Renal Cell Carcinoma (ccRCC). The VHL gene is a tumor suppressor gene and under normal conditions with normal oxygen tension, binds to Hypoxia-Inducible Factor (HIF-1 alpha) and facilitates degradation of this factor. Under hypoxic conditions and in patients having biallelic loss of function and mutation of VHL genes, HIF-1alpha is not degraded. Build up of HIF-1 alpha results in increased angiogenesis, increased tumor cell proliferation and survival, as well as metastasis. SUTENT® (Sunitinib) is a MultiKinase Inhibitor(MKI) and simultaneously targets the tumor cell wall, vascular endothelial cell wall as well as the pericyte/fibroblast/vascular/ smooth vessel cell wall and is capable of specifically binding to tyrosine kinases, inhibiting the earlier signaling events and thereby inhibits phosphorylation of VEGF receptor, PDGF receptor, FLT-3 and c-KIT. AFINITOR® (Everolimus) unlike SUTENT® does not inhibit tyrosine kinases but is a specific inhibitor of mTOR(Mammalian Target of Rapamycin) which is a serine/threonine kinase, normally activated further downstream in the signaling cascade. With the inhibition of mTOR, protein synthesis is inhibited resulting in decreased angiogenesis, cell proliferation and survival as well as decreased levels of HIF-1 alpha. Besides VHL gene mutation, several novel relatively common mutations of histone modifying and chromatin remodeling genes have been identified in clear cell RCC, with the availability of Next Generation Sequencing (NGS). Next-generation sequencing (NGS) platforms or second-generation sequencing unlike the first-generation sequencing, known as Sanger sequencing, perform massively parallel sequencing, which allows sequencing of millions of fragments of DNA from a single sample. With this high-throughput sequencing, the entire genome can be sequenced in less than 24 hours. Some of the new genes identified include PBRM1, KDM5C, SETD2 and BAP1. These are tumor suppressor genes and are located on chromosome 3p, close to the VHL gene, at the 3p locus. Mutations involving these genes in clear cell RCC, results in loss of protein expression and has been associated with advanced tumor stage, grade and poor patient outcomes.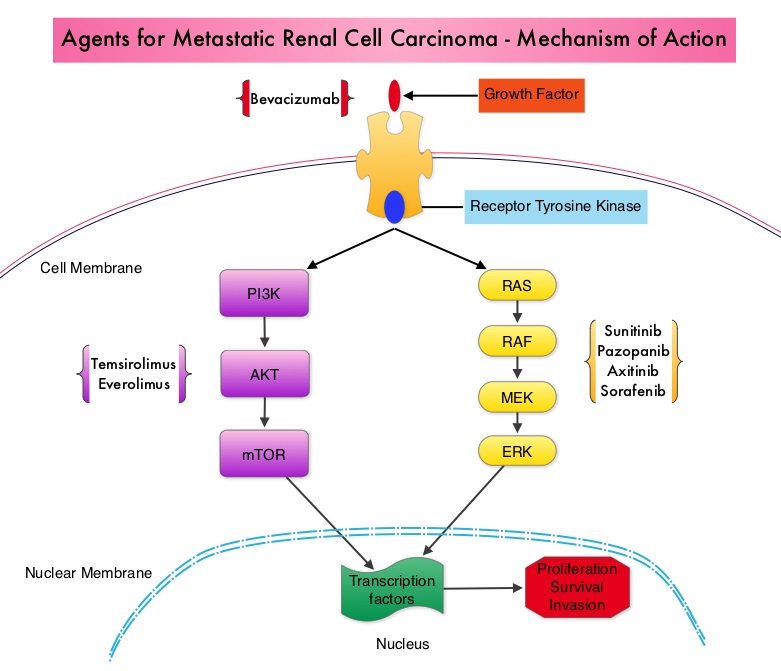
The authors in this study explored patient outcomes, based on somatic mutations and therapy given, amongst patients enrolled in the RECORD-3 trial. RECORD-3 is multicenter, randomized phase II trial which enrolled 471 treatment-naïve, metastatic, clear cell Renal Cell Carcinoma patients and compared first line AFINITOR® followed by SUTENT® at progression (N=238) with the standard sequence of first line SUTENT® followed by AFINITOR® (N=233). Using Next Generation Sequencing the authors were able to identify somatic mutations in the exons of 341 cancer related genes and associated the first line Progression Free Survival (PFS) with the tumor genotypes. They noted that 41% of the cohort of patients had PBRM1 mutations. In the group of patients receiving AFINITOR® as first line therapy, those with PBRM1 mutations had a longer median PFS compared to those who did not have PBRM1 mutations (11.1 vs 5.3 months; P=0.0031). Further, those with PBRM1 mutations, derived comparable PFS benefit from first line AFINITOR® or first line SUTENT®. In the group receiving SUTENT® as first line therapy, patients with KDM5C mutations had a longer PFS compared to those who did not have KDM5C mutations (mPFS 20.6 vs 8.4 months; P=0.0511). The authors concluded that PBRM1 and KDM5C gene mutations may predict sensitivity to mTOR or VEGFR inhibitors, in metastatic Renal Cell Carcinoma with different genomic profiles. Identification of efficacy biomarkers in a large metastatic renal cell carcinoma (mRCC) cohort through next generation sequencing (NGS): Results from RECORD-3. Hsieh J, Chen D, Wang P, et al. J Clin Oncol 33, 2015 (suppl; abstr 4509)
Late Breaking Abstract – ASCO 2015 Adjuvant Chemotherapy Improves Overall Survival in Localized High Risk Prostate Cancer
SUMMARY: Prostate cancer is the most common cancer in American men excluding skin cancer and 1 in 7 men will be diagnosed with prostate cancer during their lifetime. It is estimated that in the United States, about 220,800 new cases of prostate cancer will be diagnosed in 2015 and over 27,000 men will die of the disease. The development and progression of prostate cancer is driven by androgens. Androgen Deprivation Therapy (ADT) has therefore been the cornerstone of treatment of advanced prostate cancer and is the first treatment intervention for hormone sensitive prostate cancer. Chemotherapy is usually considered for patients who progress on hormone therapy and TAXOTERE® (Docetaxel) has been shown to improve Overall Survival (OS) of metastatic prostate cancer patients, who had progressed on Androgen Deprivation Therapy. Two previously published trials, STAMPEDE and CHAARTED have shown that TAXOTERE® in combination with Androgen Deprivaton Therapy significantly improved Overall Survival among men with newly diagnosed hormone naïve metastatic prostate cancer. Based on this information the authors hypothesized that if chemotherapy is beneficial in metastatic hormone sensitive prostate cancer, non-metastatic, hormone-sensitive, prostate cancer, should have improved outcomes with chemotherapy, as well.
RTOG 0521 is a randomized phase III trial which enrolled 612 high-risk with localized prostate cancer and 563 patients were eligible for evaluation. High risk prostate cancer was defined as 1) Patients with Gleason score of 7-8, any T-stage and PSA of 20 ng/ml or more or 2) Gleason score of 8, T2 or more and any PSA or 3) Gleason score of 9-10, any T stage and any PSA. All patients had a PSA of 150 ng/ml or less. This study was designed to detect a 51% relative reduction in the risk of death. Patients were randomized to receive Androgen Deprivation Therapy (ADT) with LHRH agonists and Radiation Therapy to a dose of 75.6 Gy (N=281) or ADT along with Radiation Therapy and TAXOTERE® (Docetaxel) 75 mg/m2 given on Day 1, every 3 weeks, for a total of 6 cycles, along with Prednisone, starting 4 weeks after the completion of Radiotherapy (N=282). Androgen Deprivation Therapy was given for 24 months and Radiation Therapy was delivered over an 8 week period. The median age was 66 years. The median PSA level was 15.1 ng/mL, 53% had Gleason scores between 9 and 10, 27% had prostate cancer with clinical T3-4 disease and 33% had node-negative disease. The primary endpoint was Overall Survival.
With a median follow up of 5.5 yrs, the 4 year Overall Survival rates were 89% for those who received ADT and Radiation Therapy (RT) compared to 93% for men treated with ADT, RT, and TAXOTERE® chemotherapy (HR=0.68; P=0.03). The 5 year Disease Free Survival rates were 66% in the ADT plus RT versus 73% in the TAXOTERE® group (HR = 0.76; P=0.05) and there was associated reduction in the incidence of distant metastasis. There were more grade 3 and 4 hematologic toxicities in the chemotherapy arm as was expected and these toxicities were manageable.
The authors concluded that this is the first phase III study to show Overall Survival benefit when TAXOTERE® is given as adjuvant chemotherapy in high risk, hormone sensitive, prostate cancer patients with localized disease. Longer follow up will determine if the role of adjuvant chemotherapy with TAXOTERE®, in this patient population will become more established.
A phase III protocol of androgen suppression (AS) and 3DCRT/IMRT versus AS and 3DCRT/IMRT followed by chemotherapy (CT) with docetaxel and prednisone for localized, high-risk prostate cancer (RTOG 0521). Sandler HM, Hu C, Rosenthal SA, et al. J Clin Oncol 33, 2015 (suppl; abstr LBA5002)
Late Breaking Abstract – ASCO 2015 IBRANCE® More Than Doubles Progression Free Survival in Hormone Receptor Positive Advanced Breast Cancer
SUMMARY: Breast cancer is the most common cancer among women in the US and about 1 in 8 women (12%) will develop invasive breast cancer during their lifetime. Approximately, 231,840 new cases of invasive breast cancer will be diagnosed in 2015 and over 40,000 women will die of the disease. Estrogen Receptor (ER) positive breast cancer cells are driven by estrogens. Tamoxifen is a nonsteroidal Selective Estrogen Receptor Modulator (SERM) and works mainly by binding to the Estrogen Receptor and thus blocks the proliferative actions of estrogen on the mammary tissue. Anastrozole and Letrozole are nonsteroidal Aromatase Inhibitors that binds reversibly to the aromatase enzyme and inhibit the conversion of androgens to estrogens in the extra-gonadal tissues.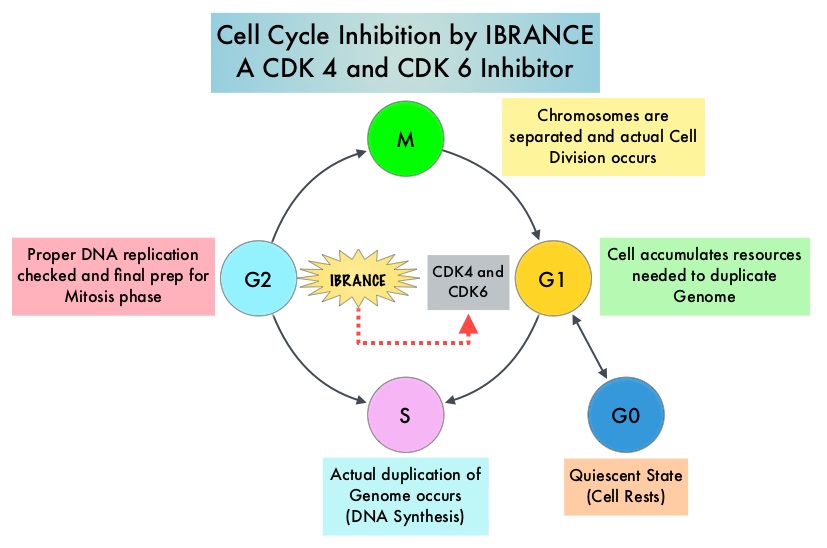 Approximately 80% of breast tumors express Estrogen Receptors and/or Progesterone Receptors and these patients are often treated with anti-estrogen therapy as first line treatment. Cyclin Dependent Kinases (CDK) play a very important role to facilitate orderly and controlled progression of the cell cycle. Genetic alterations in these kinases and their regulatory proteins have been implicated in various malignancies. Cyclin Dependent Kinases 4 and 6 (CDK4 and CDK6) phosphorylate RetinoBlastoma protein (RB) and initiate transition from the G1 phase to the S phase of the cell cycle. CDK4 and CDK6 are activated in hormone receptor positive breast cancer, promoting breast cancer cell proliferation. Further, there is evidence to suggest that endocrine resistant breast cancer cell lines depend on CDK4 for cell proliferation. IBRANCE® (Palbociclib) is a reversible, oral, selective, small molecule inhibitor of Cyclin Dependent Kinases, CDK4 and CDK6, and prevent RB1 phosphorylation. IBRANCE® is the first CDK inhibitor approved by the FDA. It exhibits synergy when combined with endocrine therapies. In an open-label, randomized, phase II study, which included treatment naïve postmenopausal women with ER-positive, HER2-negative, advanced breast cancer, IBRANCE® given along with Aromatase Inhibitor FEMARA® (Letrozole) significantly prolonged Progression Free Survival, Overall Response rate and median duration of response, compared to FEMARA® alone. Based on this data, the U. S. Food and Drug Administration on February 3, 2015 granted accelerated approval to IBRANCE® (Palbociclib), for use in combination with FEMARA® (Letrozole) in this patient population. FASLODEX® (Fulvestrant) is a selective estrogen receptor down-regulator presently indicated for the treatment of hormone receptor positive metastatic breast cancer patients, with disease progression following antiestrogen therapy.
Approximately 80% of breast tumors express Estrogen Receptors and/or Progesterone Receptors and these patients are often treated with anti-estrogen therapy as first line treatment. Cyclin Dependent Kinases (CDK) play a very important role to facilitate orderly and controlled progression of the cell cycle. Genetic alterations in these kinases and their regulatory proteins have been implicated in various malignancies. Cyclin Dependent Kinases 4 and 6 (CDK4 and CDK6) phosphorylate RetinoBlastoma protein (RB) and initiate transition from the G1 phase to the S phase of the cell cycle. CDK4 and CDK6 are activated in hormone receptor positive breast cancer, promoting breast cancer cell proliferation. Further, there is evidence to suggest that endocrine resistant breast cancer cell lines depend on CDK4 for cell proliferation. IBRANCE® (Palbociclib) is a reversible, oral, selective, small molecule inhibitor of Cyclin Dependent Kinases, CDK4 and CDK6, and prevent RB1 phosphorylation. IBRANCE® is the first CDK inhibitor approved by the FDA. It exhibits synergy when combined with endocrine therapies. In an open-label, randomized, phase II study, which included treatment naïve postmenopausal women with ER-positive, HER2-negative, advanced breast cancer, IBRANCE® given along with Aromatase Inhibitor FEMARA® (Letrozole) significantly prolonged Progression Free Survival, Overall Response rate and median duration of response, compared to FEMARA® alone. Based on this data, the U. S. Food and Drug Administration on February 3, 2015 granted accelerated approval to IBRANCE® (Palbociclib), for use in combination with FEMARA® (Letrozole) in this patient population. FASLODEX® (Fulvestrant) is a selective estrogen receptor down-regulator presently indicated for the treatment of hormone receptor positive metastatic breast cancer patients, with disease progression following antiestrogen therapy.
The PALOMA3 is double-blind, phase 3 study in which the efficacy and safety of the combination of IBRANCE® and FASLODEX® was evaluated, in premenopausal or postmenopausal women, with hormone receptor positive, HER-2 negative, advanced breast cancer, who had disease progression during prior endocrine therapy. Five hundred and twenty one (N=521) patients were randomly assigned in a 2:1 ratio to receive either FASLODEX® 500 mg IM on days 1 and 15 during cycle 1, of a 28 day cycle, and then on day 1 of each cycle thereafter, along with IBRANCE® 125 mg PO daily for 3 weeks, followed by 1 week off (N=347) or FASLODEX® and placebo (N=174). ZOLADEX® (Goserelin) was administered to premenopausal or perimenopausal patients for the duration of study treatment, starting at least 4 weeks before randomization and continuing every 28 days. The median age was 57 years. One previous line of chemotherapy for metastatic disease was allowed and 79% were post-menopausal, 60% had visceral disease and 33% of the patients had prior chemotherapy for advanced disease. The primary endpoint was Progression Free Survival (PFS) and secondary endpoints included Overall Survival (OS), Response Rates, safety and tolerability. At the time of the preplanned interim analysis, the median Progression Free Survival was 9.2 months in the FASLODEX® / IBRANCE® group and 3.8 months in the FASLODEX® /placebo group (HR=0.422; P<0.000001). This PFS benefit was observed across all prespecified patient subgroups, regardless of menopausal status. The most common adverse events in the IBRANCE® group were neutropenia (78.8% vs 3.5%) and fatigue (38.0% vs 26.7%). The incidence of febrile neutropenia was very rare (0.6%) and similar in both treatment groups. Treatment discontinuation rate due to adverse events was 2% in the IBRANCE® group and 1.7% in the placebo group. The authors concluded that IBRANCE® in combination with FASLODEX® more than doubled the Progression Free Survival in advanced breast cancer patients, with hormone receptor positive and HER-2 negative disease, who had progressed on prior endocrine therapy. This study has reinforced the importance of CDK4 and CDK6, as key targets for hormone receptor positive breast cancer. Palbociclib in Hormone Receptor Positive Advanced Breast Cancer. Turner NC, Ro J, Andre F, et al. June 1, 2015DOI: 10.1056/NEJMoa1505270
Late Breaking Abstract – ASCO 2015 KEYTRUDA®, an Anti PD-1 Antibody for Advanced Head and Neck Cancer
SUMMARY: The American Cancer Society estimates that 59,340 people will be diagnosed with Head and Neck cancer in 2015 and 12,290 patients will die of the disease. Patients with recurrent/metastatic Squamous Cell Carcinoma of the Head and Neck (SCCHN) have a poor prognosis with a median Overall Survival (OS) of about 13 months with first line therapy and about 6 months or less with later lines of therapy. The treatment paradigm for solid tumors has been rapidly evolving with a better understanding of the Immune checkpoints. Immune checkpoints are cell surface inhibitory proteins/receptors that are expressed on activated T cells. They harness the immune system and prevent uncontrolled immune reactions. Survival of cancer cells in the human body may be to a significant extent, related to their ability to escape immune surveillance, by inhibiting T lymphocyte activation. The T cells of the immune system therefore play a very important role in modulating the immune system. Under normal circumstances, inhibition of an intense immune response and switching off the T cells of the immune system, is an evolutionary mechanism and is accomplished by Immune checkpoints or gate keepers. With the recognition of Immune checkpoint proteins and their role in suppressing antitumor immunity, antibodies are being developed that target the membrane bound inhibitory Immune checkpoint proteins/receptors such as CTLA-4 (Cytotoxic T-Lymphocyte Antigen 4), also known as CD152, PD-1(Programmed cell Death-1), etc. By doing so, one would expect to unleash the T cells, resulting in T cell proliferation, activation and a therapeutic response. The first Immune checkpoint protein to be clinically targeted was CTLA-4. YERVOY® (Ipilimumab), an antibody that blocks Immune checkpoint protein/receptor CTLA- 4, has been shown to prolong overall survival in patients with previously treated, unresectable or metastatic melanoma. KEYTRUDA® (Pembrolizumab) is a fully humanized, Immunoglobulin G4, monoclonal antibody, that binds to the PD-1 receptor and blocks its interaction with ligands PD-L1 and PD-L2, thereby undoing PD-1 pathway-mediated inhibition of the immune response and unleashing the tumor-specific effector T cells. The FDA granted accelerated approval to KEYTRUDA® in September 2014, for the treatment of patients with unresectable or metastatic melanoma and disease progression following YERVOY® and, if BRAF V600 mutation positive, a BRAF inhibitor. The activity of KEYTRUDA® as a single agent in advanced SCCHN patients, was previously published and was noted in PD-L1 positive tumors, regardless of the Human PapillomaVirus (HPV) status. The Overall Response Rate in this patient group was 20% and 29% of patients had stable disease. The authors in this study reported the efficacy of once every three week dose of KEYTRUDA®, in a larger expansion cohort of KEYNOTE 012 study. In this study, 132 patients with recurrent/metastatic SCCHN were enrolled, regardless of their PD-L1 expression or HPV status. These patients received a fixed dose of KEYTRUDA® 200 mg IV, every 3 weeks and patients were evaluated every 8 weeks with radiographic imaging. The mean age was 59 years and 57% of the patients had 2 or more lines of therapy for recurrent disease. Treatment was continued until disease progression. The primary end point was Overall Response Rate (ORR) and secondary endpoints included Progression Free Survival (PFS) and Overall Survival (OS). The Overall Response Rate was 25% and stable disease was noted in an additional 25% of the patients. This amounted to a disease control rate of 50%. Patients with HPV-positive disease had a response rate of 20.6% and patients with HPV-negative disease had a response rate of 27.2%, suggesting that KEYTRUDA® was active in both subgroups of patients. Serious toxicities were reported in fewer than 10% of patients and the most common adverse event was fatigue (15.2%). The authors concluded that KEYTRUDA® given every 3 weeks was well tolerated and demonstrated a meaningful response rate in a heavily pretreated population of patients, with recurrent/metastatic SCCHN. Evaluation of PD-L1 status for this patient group is ongoing. Antitumor activity and safety of pembrolizumab in patients (pts) with advanced squamous cell carcinoma of the head and neck (SCCHN): Preliminary results from KEYNOTE-012 expansion cohort. Seiwert TY, Haddad RI, Gupta S, et al. J Clin Oncol 33, 2015 (suppl; abstr LBA6008)</s
Immune checkpoints are cell surface inhibitory proteins/receptors that are expressed on activated T cells. They harness the immune system and prevent uncontrolled immune reactions. Survival of cancer cells in the human body may be to a significant extent, related to their ability to escape immune surveillance, by inhibiting T lymphocyte activation. The T cells of the immune system therefore play a very important role in modulating the immune system. Under normal circumstances, inhibition of an intense immune response and switching off the T cells of the immune system, is an evolutionary mechanism and is accomplished by Immune checkpoints or gate keepers. With the recognition of Immune checkpoint proteins and their role in suppressing antitumor immunity, antibodies are being developed that target the membrane bound inhibitory Immune checkpoint proteins/receptors such as CTLA-4 (Cytotoxic T-Lymphocyte Antigen 4), also known as CD152, PD-1(Programmed cell Death-1), etc. By doing so, one would expect to unleash the T cells, resulting in T cell proliferation, activation and a therapeutic response. The first Immune checkpoint protein to be clinically targeted was CTLA-4. YERVOY® (Ipilimumab), an antibody that blocks Immune checkpoint protein/receptor CTLA- 4, has been shown to prolong overall survival in patients with previously treated, unresectable or metastatic melanoma. KEYTRUDA® (Pembrolizumab) is a fully humanized, Immunoglobulin G4, monoclonal antibody, that binds to the PD-1 receptor and blocks its interaction with ligands PD-L1 and PD-L2, thereby undoing PD-1 pathway-mediated inhibition of the immune response and unleashing the tumor-specific effector T cells. The FDA granted accelerated approval to KEYTRUDA® in September 2014, for the treatment of patients with unresectable or metastatic melanoma and disease progression following YERVOY® and, if BRAF V600 mutation positive, a BRAF inhibitor. The activity of KEYTRUDA® as a single agent in advanced SCCHN patients, was previously published and was noted in PD-L1 positive tumors, regardless of the Human PapillomaVirus (HPV) status. The Overall Response Rate in this patient group was 20% and 29% of patients had stable disease. The authors in this study reported the efficacy of once every three week dose of KEYTRUDA®, in a larger expansion cohort of KEYNOTE 012 study. In this study, 132 patients with recurrent/metastatic SCCHN were enrolled, regardless of their PD-L1 expression or HPV status. These patients received a fixed dose of KEYTRUDA® 200 mg IV, every 3 weeks and patients were evaluated every 8 weeks with radiographic imaging. The mean age was 59 years and 57% of the patients had 2 or more lines of therapy for recurrent disease. Treatment was continued until disease progression. The primary end point was Overall Response Rate (ORR) and secondary endpoints included Progression Free Survival (PFS) and Overall Survival (OS). The Overall Response Rate was 25% and stable disease was noted in an additional 25% of the patients. This amounted to a disease control rate of 50%. Patients with HPV-positive disease had a response rate of 20.6% and patients with HPV-negative disease had a response rate of 27.2%, suggesting that KEYTRUDA® was active in both subgroups of patients. Serious toxicities were reported in fewer than 10% of patients and the most common adverse event was fatigue (15.2%). The authors concluded that KEYTRUDA® given every 3 weeks was well tolerated and demonstrated a meaningful response rate in a heavily pretreated population of patients, with recurrent/metastatic SCCHN. Evaluation of PD-L1 status for this patient group is ongoing. Antitumor activity and safety of pembrolizumab in patients (pts) with advanced squamous cell carcinoma of the head and neck (SCCHN): Preliminary results from KEYNOTE-012 expansion cohort. Seiwert TY, Haddad RI, Gupta S, et al. J Clin Oncol 33, 2015 (suppl; abstr LBA6008)</s
ASCO 2015 Selective Internal Radiation Therapy with Y-90 Improves Outcomes in Metastatic Colorectal Cancer
SUMMARY:The American Cancer Society estimates that approximately 133,000 new cases of ColoRectal Cancer (CRC) will be diagnosed in the United States in 2015 and close to 50,000 are expected to die of the disease. Approximately 15-25% of the patients with CRC present with metastatic disease at the time of diagnosis (synchronous metastases) and 50-60% of the patients with CRC will develop metastatic disease during the course of their illness. About 10-20% of the patients with liver metastases have resectable disease, which may translate into long term survival. CRC patients with synchronous metastases tend to have more extensive disease with bilobar liver involvement. With the availability of more effective chemotherapy regimens and targeted systemic interventions, the median survival of CRC patients with metastatic disease has increased from 6 months in the 1990’s to 24 months. Selective Internal Radiation Therapy (SIRT) or RadioEmbolization using radioisotope Yttrium-90 (Y-90) coated resin particles, a pure beta emitter, has demonstrated significant benefit for patients with unresectable liver metastases, in previously published studies. Y-90 resin microspheres are no bigger in diameter than a human hair and are introduced into the hepatic artery by initially accessing the femoral artery. The blood supply to the liver tumors is via the hepatic artery and these tumors tend to be hypervascular. The Y-90 resin microspheres become preferentially lodged in the narrow capillaries that surround liver tumors and selectively deliver a high dose of short-range beta radiation to the liver tumors. The physical properties of Y-90 resin microspheres facilitate even distribution of radioactivity within and around the liver metastases. SIRFLOX is an International, multi-center, open-label, randomized phase III study, which evaluated the efficacy and safety of combining modified FOLFOX6 (Oxaliplatin, 5-FU and Leucovorin) chemotherapy regimen with or without AVASTIN® (Bevacizumab) with SIRT, using Y-90 resin microspheres, as first line treatment in patients with unresectable liver only or liver dominant metastatic ColoRectal Cancer (mCRC). The randomization included 530 patients of whom 263 patients received mFOLFOX6 with or without AVASTIN® (Group A) and 267 patients received mFOLFOX6 + SIRT administered once with cycle 1, with or without AVASTIN® (Group B), with the treatment given until disease progression. Patients were stratified based on the extent of liver involvement (25% or less versus more than 25%), presence of extra hepatic disease (liver only versus liver dominant disease) and treatment with AVASTIN®, which was at the discretion of the attending physician. Forty percent of the patients had extra hepatic disease. The primary endpoint was Progression Free Survival (PFS). With a median follow up of 36.1 months, the median PFS in the liver was 12.6 months versus 20.5 months in Group A versus Group B respectively (HR=0.69; P=0.002). The hepatic Response Rate was 68.8% versus 78.7% (P=0.042), with a Complete Response Rate of 1.9% versus 6.0% (P=0.02) in Groups A and B respectively. Even though hematologic and gastrointestinal adverse events were higher in the SIRT group, the toxicity levels were acceptable. The authors concluded that the addition of SIRT to chemotherapy resulted in a 7.9 month improvement in Progression Free Survival in the liver, for patients with unresectable metastatic ColoRectal cancer (mCRC), with a 31% reduction in the risk of tumor progression in the liver. With the liver being the most common site of spread in patients with metastatic CRC, this study provides Level One evidence to support the use of SIRT in combination with chemotherapy in this patient group. SIRFLOX: Randomized phase III trial comparing first-line mFOLFOX6 ± bevacizumab (bev) versus mFOLFOX6 + selective internal radiation therapy (SIRT) ± bev in patients (pts) with metastatic colorectal cancer (mCRC). Gibbs P, Heinemann V, Sharma NK, et al. J Clin Oncol 33, 2015 (suppl; abstr 3502)</s
SIRFLOX is an International, multi-center, open-label, randomized phase III study, which evaluated the efficacy and safety of combining modified FOLFOX6 (Oxaliplatin, 5-FU and Leucovorin) chemotherapy regimen with or without AVASTIN® (Bevacizumab) with SIRT, using Y-90 resin microspheres, as first line treatment in patients with unresectable liver only or liver dominant metastatic ColoRectal Cancer (mCRC). The randomization included 530 patients of whom 263 patients received mFOLFOX6 with or without AVASTIN® (Group A) and 267 patients received mFOLFOX6 + SIRT administered once with cycle 1, with or without AVASTIN® (Group B), with the treatment given until disease progression. Patients were stratified based on the extent of liver involvement (25% or less versus more than 25%), presence of extra hepatic disease (liver only versus liver dominant disease) and treatment with AVASTIN®, which was at the discretion of the attending physician. Forty percent of the patients had extra hepatic disease. The primary endpoint was Progression Free Survival (PFS). With a median follow up of 36.1 months, the median PFS in the liver was 12.6 months versus 20.5 months in Group A versus Group B respectively (HR=0.69; P=0.002). The hepatic Response Rate was 68.8% versus 78.7% (P=0.042), with a Complete Response Rate of 1.9% versus 6.0% (P=0.02) in Groups A and B respectively. Even though hematologic and gastrointestinal adverse events were higher in the SIRT group, the toxicity levels were acceptable. The authors concluded that the addition of SIRT to chemotherapy resulted in a 7.9 month improvement in Progression Free Survival in the liver, for patients with unresectable metastatic ColoRectal cancer (mCRC), with a 31% reduction in the risk of tumor progression in the liver. With the liver being the most common site of spread in patients with metastatic CRC, this study provides Level One evidence to support the use of SIRT in combination with chemotherapy in this patient group. SIRFLOX: Randomized phase III trial comparing first-line mFOLFOX6 ± bevacizumab (bev) versus mFOLFOX6 + selective internal radiation therapy (SIRT) ± bev in patients (pts) with metastatic colorectal cancer (mCRC). Gibbs P, Heinemann V, Sharma NK, et al. J Clin Oncol 33, 2015 (suppl; abstr 3502)</s
Immediate ADT Confers Survival Benefit in Prostate Cancer Patients with “Biochemical Recurrence”
SUMMARY: Prostate cancer is the most common cancer in American men excluding skin cancer and 1 in 7 men will be diagnosed with prostate cancer during their lifetime. It is estimated that in the United States, about 220,800 new cases of prostate cancer will be diagnosed in 2015 and over 27,000 men will die of the disease. The major source of PSA (Prostate Specific Antigen) is the prostate gland and the PSA levels are therefore undetectable within 6 weeks after Radical Prostatectomy. Similarly, following Radiation Therapy, there is a gradual decline in PSA before reaching a post treatment nadir. A detectable PSA level after Radical Prostatectomy, or a rising PSA level following Radiation Therapy, is considered PSA failure or biochemical recurrence.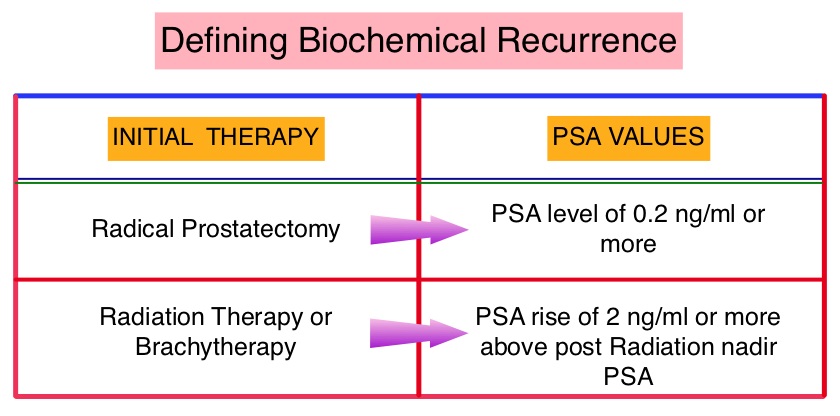 The American Urological Association suggested that a PSA of 0.2 ng/mL or higher after Radical Prostatectomy, defines PSA failure or relapse. A PSA rise of 2 ng/ml or more above post Radiation Therapy nadir is considered PSA failure or relapse. Approximately 35% of the patients with prostate cancer will experience PSA only relapse within 10 years of their primary treatment and a third of these patients will develop documented metastatic disease within 8 years following PSA only relapse. The development and progression of prostate cancer is driven by androgens. Androgen Deprivation Therapy (ADT) has therefore been the cornerstone of treatment of advanced prostate cancer and is the first treatment intervention for hormone sensitive prostate cancer. The appropriate time (immediate versus delayed) to start Androgen Deprivation Therapy (ADT) in patients with prostate cancer with rising Prostate-Specific Antigen (PSA), as the only sign of relapse, has remained unclear. This has been partly due to lack of patient accruals and patient reluctance to be randomized, in these clinical trials.
The American Urological Association suggested that a PSA of 0.2 ng/mL or higher after Radical Prostatectomy, defines PSA failure or relapse. A PSA rise of 2 ng/ml or more above post Radiation Therapy nadir is considered PSA failure or relapse. Approximately 35% of the patients with prostate cancer will experience PSA only relapse within 10 years of their primary treatment and a third of these patients will develop documented metastatic disease within 8 years following PSA only relapse. The development and progression of prostate cancer is driven by androgens. Androgen Deprivation Therapy (ADT) has therefore been the cornerstone of treatment of advanced prostate cancer and is the first treatment intervention for hormone sensitive prostate cancer. The appropriate time (immediate versus delayed) to start Androgen Deprivation Therapy (ADT) in patients with prostate cancer with rising Prostate-Specific Antigen (PSA), as the only sign of relapse, has remained unclear. This has been partly due to lack of patient accruals and patient reluctance to be randomized, in these clinical trials.
The authors conducted this randomized, prospective, phase III trial, to determine if immediate intervention with Androgen Deprivation Therapy (ADT) would improve Overall Survival (OS), compared with delayed ADT, in prostate cancer patients with PSA relapse, following definitive therapy, or in asymptomatic men not suitable for definitive therapy at the time of diagnosis. This analysis combined prostate cancer patients with PSA relapse enrolled in two separate studies. Two hundred and ninety three (N=293) eligible patients were randomly assigned 1:1 to immediate Androgen Deprivation Therapy (N= 142) or delayed ADT (N=151). The primary endpoint was unadjusted Overall Survival. Secondary endpoints included cancer-specific survival and time to clinical progression. The median follow up was 5 years. There was a statistically significant improvement in the Overall Survival, with a 45% reduction in the risk for death, for those receiving immediate ADT compared with the delayed treatment group (HR=0.55; P=0.05). Further, with immediate ADT, there was a statistically significant delay in the time to first local progression (HR= 0.51; P=0.001) as well as time to first metastatic disease (HR=0.54; P=0.018). The authors concluded that immediate Androgen Deprivation Therapy significantly improved Overall Survival and time to clinical progression for prostate cancer patients with PSA relapse, after definitive therapy. This benefit however must be weighed against the risks associated with long term Androgen Deprivation Therapy. TROG 03.06 and VCOG PR 01-03: The “Timing Of Androgen Deprivation therapy in prostate cancer patients with a rising PSA (TOAD)” collaborative randomised phase III trial. Duchesne GM, Bassett J, D’Este C, et al. J Clin Oncol 33, 2015 (suppl; abstr 5007)
Late Breaking Abstract – ASCO 2015 IMBRUVICA® in Combination with BR Regimen Shows Significant Benefit in Relapsed CLL patients
SUMMARY: The American Cancer Society estimates that approximately 14,620 new cases of Chronic Lymphocytic Leukemia (CLL) will be diagnosed in 2015 and approximately 4650 patients will die from the disease. CLL is a disease of the elderly and the average age at the time of diagnosis is 72 years. There are two main types of lymphocytes, B and T lymphocytes/cells. B-cell CLL is the most common type of leukemia in adults. Normal B-cell activation and proliferation is dependent on B-cell receptor (BCR) signaling. This signaling is also important for initiation and progression of B-cell lymphoproliferative disorders. Bruton’s Tyrosine Kinase (BTK) is a member of the Tec family of kinases, downstream of the B-cell receptor and is predominantly expressed in B-cells. It is a mediator of B-cell receptor signaling in normal and transformed B-cells. Following binding of antigen to the B-Cell Receptor, kinases such as Syk (Spleen Tyrosine Kinase), Lyn (member of the Src family of protein tyrosine kinases) and BTK (Bruton’s Tyrosine Kinase) are activated, with subsequent propagation through PI3K/Akt, MAPK, and NF-κB pathways. This results in B-cell activation and proliferation. IMBRUVICA® (Ibrutinib) is an oral, irreversible inhibitor of BTK and inhibits cell proliferation and promotes programmed cell death (Apoptosis) by blocking B-cell activation and signaling. The FDA initially granted accelerated approval to IMBRUVICA® in February 2014 for previously treated patients with CLL and this was followed by full FDA approval and a new treatment indication for high-risk CLL patients with 17p deletions, in July 2014. Previously published studies had shown significant Response Rates and and Event-Free Survival with BR (Bendamustine-TREANDA® and Rituximab-RITUXAN®) in FLUDARA® (Fludarabine) refractory patients, with Chronic Lymphocytic Leukemia.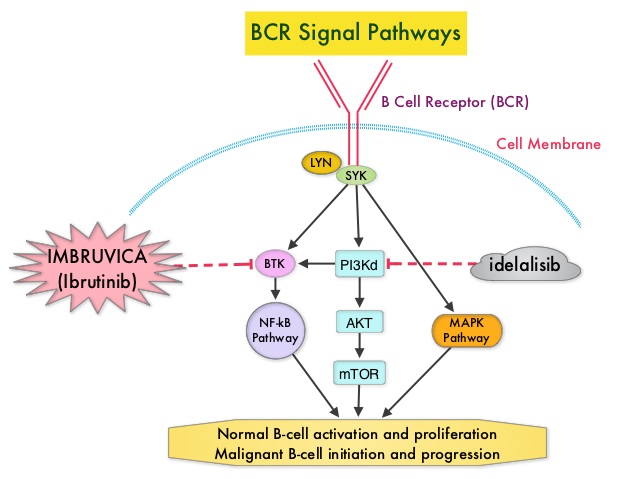
The HELIOS study is a double-blind, randomized, phase III trial which evaluated the benefit of combining IMBRUVICA® with BR compared to placebo plus BR, in patients with previously treated, relapsed/refractory Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma. In this study, of the 578 randomized patients, 289 patients received a maximum of six cycles of BR with IMBRUVICA® 420 mg PO daily and 289 patients received BR with placebo. The median patient age was 64 years, patients had received a median of two prior therapies and 38% of the patients had Rai Stage III/IV disease. Patients with 17p deletions in more than >20% of cells, were excluded. The planned six cycles of BR were completed by 83% in the IMBRUVICA® group and 78% in the placebo group. The primary endpoint was Progression Free Survival (PFS). Secondary endpoints included Overall Survival (OS) and Overall Response Rate (ORR). Following an interim analysis, this study was unblinded as there was a significant PFS benefit with IMBRUVICA® and patients receiving placebo, were allowed to cross over to the IMBRUVICA® group, per study protocol,. Thirty one percent (31%) of the patients in the BR plus placebo group with confirmed progressive disease crossed over to receive BR plus IMBRUVICA®. At a median follow up of 17.2 months, the PFS in the IMBRUVICA® plus BR group was not yet reached whereas the PFS was 13.3 months for patients receiving placebo plus BR (HR=0.203; P<0.0001). This PFS benefit was seen across subgroups of high-risk patients as well. The ORR was 82.7% in the IMBRUVICA® plus BR group compared to 67.8% in the placebo plus BR group (P <0.0001). Complete Response (CR) rates which included CR with incomplete blood count recovery were 10.4% versus 2.8% with IMBRUVICA® and placebo, respectively. The median OS was not reached. The incidence of most adverse events were comparable between the two treatment groups and the most frequent side effects were neutropenia affecting about 55% of the patients and nausea experienced by about 35% of the patients. The authors concluded that IMBRUVICA® plus BR resulted in an 80% reduction in the risk of disease progression, as well as improved Overall Response Rates, compared to placebo plus BR. This triplet combination of IMBRUVICA®, TREANDA® and RITUXAN® should therefore be considered an important treatment option for patients with previously treated Chronic Lymphocytic Leukemia and Small Lymphocytic Lymphoma. Ibrutinib combined with bendamustine and rituximab (BR) in previously treated chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL): first results from a randomized, double-blind, placebo-controlled, phase III study. Chanan-Khan AAA, Cramer P, Demirkan F, et al. J Clin Oncol. 2015;33 (suppl; abstr LBA7005).
Daily Aspirin May Improve Survival after Diagnosis of Colorectal Cancer
SUMMARY:The American Cancer Society estimates that approximately 133,000 new cases of ColoRectal Cancer (CRC) will be diagnosed in the United States in 2015 and close to 50,000 are expected to die of the disease. Several epidemiological studies as well as randomized controlled trials have shown that Aspirin reduces the incidence of ColoRectal Cancer (CRC) and CRC associated mortality. Platelets have long been implicated in the mechanism of tumor metastases. More recent data suggests that platelets may play a role in tumorigenesis as well, through the release of angiogenic and growth factors due to overexpression of COX-2. Daily low dose Aspirin inhibits COX-1 and COX-2. 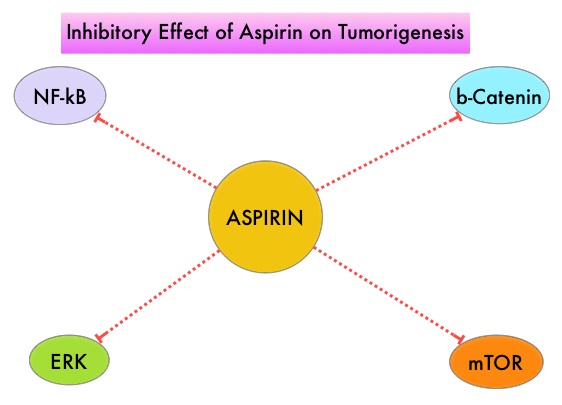 It is postulated that Aspirin also works by COX-independent mechanisms such as, the inhibition of NF-kB and Wnt/ β-catenin signaling, which may play a role in its chemopreventive properties. Even though the benefits of Aspirin in the primary prevention of CRC remains well established, the role of Aspirin in secondary prevention in patients with CRC is unclear. The authors conducted this trial to evaluate the association between Aspirin use after diagnosis of CRC with CRC-Specific Survival (CSS) and Overall Survival (OS) in the largest group of patients ever studied. The study authors in this retrospective study identified 25,644 patients in the Cancer Registry of Norway, diagnosed with ColoRectal Cancer (CRC) from 2004 through 2011. Using the Norwegian Prescription Database, the authors were then able to establish that 6,109 patients in this large cohort had documented exposure to Aspirin. Exposure to Aspirin was defined as a prescription for more than 6 months of Aspirin following a diagnosis of CRC. The median follow up was 2.2 years. The authors performed a multivariate regression analysis controlling for age, gender, tumor stage, tumor differentiation and noted that exposure to Aspirin post-diagnosis, independently improved ColoRectal Cancer (CRC) -Specific Survival (HR=0.75; P<0.001) and Overall Survival (HR=0.86; P<0.001). The authors concluded that in this large group of unselected ColoRectal Cancer (CRC) patients, exposure to Aspirin after the diagnosis of CRC is independently associated with improved Colorectal Cancer-Specific Survival and Overall Survival. They added that because of the risk of bleeding, the risk–benefit should be assessed before Aspirin is routinely recommended to this patient population. Impact of aspirin as secondary prevention in an unselected cohort of 25,644 patients with colorectal cancer: A population-based study. Bains S, Mahic M, Cvancarova M, et al. J Clin Oncol 33, 2015 (suppl; abstr 3504)
It is postulated that Aspirin also works by COX-independent mechanisms such as, the inhibition of NF-kB and Wnt/ β-catenin signaling, which may play a role in its chemopreventive properties. Even though the benefits of Aspirin in the primary prevention of CRC remains well established, the role of Aspirin in secondary prevention in patients with CRC is unclear. The authors conducted this trial to evaluate the association between Aspirin use after diagnosis of CRC with CRC-Specific Survival (CSS) and Overall Survival (OS) in the largest group of patients ever studied. The study authors in this retrospective study identified 25,644 patients in the Cancer Registry of Norway, diagnosed with ColoRectal Cancer (CRC) from 2004 through 2011. Using the Norwegian Prescription Database, the authors were then able to establish that 6,109 patients in this large cohort had documented exposure to Aspirin. Exposure to Aspirin was defined as a prescription for more than 6 months of Aspirin following a diagnosis of CRC. The median follow up was 2.2 years. The authors performed a multivariate regression analysis controlling for age, gender, tumor stage, tumor differentiation and noted that exposure to Aspirin post-diagnosis, independently improved ColoRectal Cancer (CRC) -Specific Survival (HR=0.75; P<0.001) and Overall Survival (HR=0.86; P<0.001). The authors concluded that in this large group of unselected ColoRectal Cancer (CRC) patients, exposure to Aspirin after the diagnosis of CRC is independently associated with improved Colorectal Cancer-Specific Survival and Overall Survival. They added that because of the risk of bleeding, the risk–benefit should be assessed before Aspirin is routinely recommended to this patient population. Impact of aspirin as secondary prevention in an unselected cohort of 25,644 patients with colorectal cancer: A population-based study. Bains S, Mahic M, Cvancarova M, et al. J Clin Oncol 33, 2015 (suppl; abstr 3504)
