SUMMARY: Thrombotic Thrombocytopenic Purpura (TTP), Hemolytic Uremic Syndrome (HUS) and Atypical Hemolytic Uremic Syndrome (aHUS) are life-threatening Thrombotic MicroAngiopathies (TMAs) associated with systemic microvascular thrombosis, MicroAngiopathic Hemolytic Anemia (MAHA), thrombocytopenia and organ failure. Even though their clinical presentation has some similarities, they are distinct entities with different pathophysiology and hence managed differently. Patients with TTP have either severe deficiency of ADAMTS13 (A Disintegrin And Metalloproteinase with a ThromboSpondin type 1 motif, member 13) secondary to anti-ADAMTS13 autoantibodies or rarely due to ADAMTS13 gene mutations. The physiological role of ADAMTS13 is to prevent intravascular platelet thrombosis. ADAMTS13 accomplishes this by cleaving ultralarge von Willebrand Factor multimers (which bind to platelets and induce aggregation), thereby mitigating the tendency of von Willebrand Factor (vWF) and platelets to form aggregates in normal microcirculation. Deficiency of ADAMTS13 causes vWF-platelet aggregation in the arterioles and capillaries, characteristic of TTP, resulting in tissue ischemia from microthrombi and end organ damage. Thus the microthrombi in TTP are platelets bound to vWF and not to fibrinogen. Rapid initiation of Plasma Exchange, the frontline therapy in patients with TTP, removes the anti-ADAMTS13 autoantibodies and ultra large vWF multimers and replenishes ADAMTS13. Immunosuppressive therapy with glucocorticoids and RITUXAN® (Rituximab) inhibits anti-ADAMTS13 autoantibody formation, by targeting the B lymphocytes. These interventions have significantly improved the survival rate among patients with TTP. Despite these advances with the use of Plasma Exchange, approximately 10-20% of the patients with TTP will succumb to their disease.
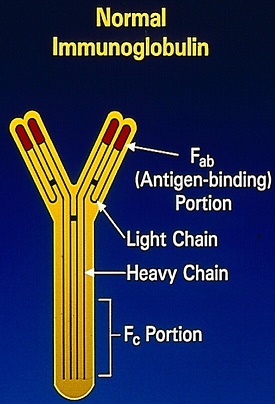
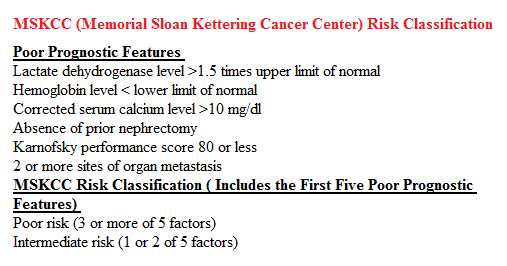
Caplacizumab is an anti-von Willebrand Factor, humanized, single-variable-domain immunoglobulin (Nanobody), directed against the A1 domain of von Willebrand Factor and prevents the interaction of vWF with the platelet glycoprotein Ib-IX receptor. TITAN is an international, multicenter, phase II, randomized, placebo-controlled study, designed to assess the efficacy and safety of Caplacizumab given as an adjunct to Plasma Exchange, in patients with acquired TTP. Seventy five patients (N=75) were randomized in a 1:1 ratio to receive Plasma Exchange plus either Caplacizumab 10 mg subcutaneous or placebo, daily. The mean age was 42 years and the mean platelet count was 24,600 per cubic millimeter. Majority of the patients in both groups received concomitant glucocorticoids and 23% of the patients in the placebo group received RITUXAN® during daily Plasma Exchange compared 6% in the Caplacizumab group. The primary end point was the time to response, defined as normalization of the platelet count (150,000 per cubic millimeter or higher) and a Lactate DeHydrogenase (LDH) level that was no more than twice the upper limit of the normal range. Secondary end points included TTP exacerbations and relapses.
It was noted that the median time to a response was significantly reduced with Caplacizumab as compared with placebo (39% reduction in median time, P=0.005). The mean number of Plasma Exchange days was lower with Caplacizumab (5.9 versus 7.9 days), the mean volume of Plasma administered was lower with Caplacizumab (19.9L versus 28.3L), normalization of LDH and creatinine occurred more rapidly with Caplacizumab and Complete Remissions after initial course of Plasma Exchange was more common in the Caplacizumab group (81% versus 46%), when compared to the placebo group. Mild to moderate bleeding was more common with Caplacizumab than with placebo (54% versus 38%).
The authors concluded that the addition of Caplacizumab to Plasma Exchange induces a faster resolution of acute TTP compared with placebo and Caplacizumab maintained a platelet-protective effect during the treatment period. Caplacizumab for Acquired Thrombotic Thrombocytopenic Purpura. Peyvandi F, Scully M, Hovinga JK, et al. for the TITAN Investigators. N Engl J Med 2016; 374:511-522