SUMMARY: Secondary hypogammaglobulinemia is a common immune defect in malignancies such as Chronic Lymphocytic Leukemia, Multiple Myeloma and Non-Hodgkin B cell lymphomas. Approximately 20-70% of these patients may experience hypogammaglobulinemia during the course of their illness. Secondary hypogammaglobulinemia generally correlates with duration and stage of the disease and there is a direct relationship between the frequency/severity of infections and low IgG levels. The infection risk may be further exacerbated by treatment induced hypogammaglobulinemia.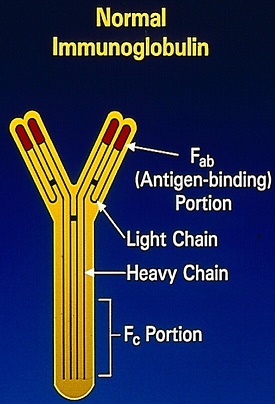
IntraVenous Immune globulin (IVIg) is a purified plasma fraction and contains more than 95% unmodified Immunoglobulin G (IgG). It is derived from large donor pools and is often recommended for patients with hypogammaglobulinemia, to reduce the risk of serious infection. With the recognition of serious IVIg-associated ThromboEmbolic Events (TEEs) dating back to the 1980’s, the FDA in 2013 mandated boxed warning for IVIg products. The TEE risk has been attributed to increased blood viscosity secondary to erythrocyte aggregation following administration of IVIg, resulting in stasis and thrombosis, platelet activation by exogenous IgG, arterial vasospasm and other plasma components such as coagulation factor XIa, that is not completely removed in some IVIg manufacturing processes. However, it is not clear if the TEEs are directly attributable to the IVIg itself or whether other risk factors such as patient’s age, disease state or other factors play a role.
The authors in this study conducted a retrospective review of data from the Surveillance, Epidemiology and End Results (SEER) cancer registries for Chronic Lymphocytic Leukemia (CLL) and Multiple Myeloma (MM) patients, linked to Medicare claims and enrollment data. This study included CLL and Myeloma patients (N=2724), 66 years or older, who were new users of IVIg and this group was propensity matched to non recipients of IVIg (N=8035). Propensity matching allowed comparison of groups across measured demographic and clinical characteristics and other variables. The primary endpoint was the occurrence of serious arterial ThromboEmbolic Event (TEE), defined as hospitalization for Acute Myocardial Infarction or Ischemic Stroke. Secondary endpoints included venous TEE (hospitalization for Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE). Based on previously published studies, the authors hypothesized that the prothrombotic effects of IVIg would most likely be acute but could last for as long as 1 month after an IVIg infusion.
It was noted that patients receiving IVIg were significantly more likely to develop a TEE such as Acute Myocardial Infarction or Stroke within the first 24 hours compared to IVIg nonrecipients (HR=3.40). This arterial thrombotic risk declined during the following 30 days. There was however, no significant increase in venous thrombotic events during the first 30 days after IVIg infusion. The risk for any ThromboEmbolic Events (TEEs) increased with age during the first 30 days following IVIg therapy (P=0.03), but was not associated with the type or duration of malignancy, history cardiovascular disease, history of venous thromboembolism or IVIg brand.
It was concluded that based on this study, arterial thrombotic events (Myocardial Infarction and Stroke) are likely to occur within the first 24 hours following IVIg administration, in patients with immunodeficiency, secondary to Chronic Lymphocytic Leukemia or Multiple Myeloma and this thrombotic risk is more common with increasing patient age. Clinicians should therefore weigh the risk/benefits with IVIg use and elderly patients should be well hydrated and closely monitored for the first 24 hours following IVIg infusion. Intravenous immune globulin and thromboembolic adverse events in patients with hematologic malignancy. Eric M. Ammann EM, Jones MP, Link BK, et al. Blood 2016; 127:200-207

