SUMMARY: Cancer in general is a disease of the elderly with two thirds of all cancers and close to three fourths of cancer mortality occurring in individuals 65 years of age or older. Elderly patients are less likely to be offered chemotherapy, as these patients are at an increased risk for chemotherapy related toxicity, compared to their younger counterparts. This may be due to a variety of reasons including decreased bone marrow reserve with aging and an increased risk of chemotherapy-related myelosuppression, inability to endure treatment due to decreased physiologic reserves, as well as impaired clearance of chemotherapy drugs due to decreased renal function. Further, cognitive and hearing impairment along with a poor support system also play an important role in the elderly, not seeking medical care, in a timely manner. Unfortunately, elderly patients are often excluded from participating in clinical trials, which makes it even more difficult to weigh the risks and benefits of chemotherapy in this patient group. Patient Performance Status is often taken into consideration to predict tolerance to chemotherapy as well as outcomes, although it remains unclear if this is a valid predictor of toxicity in elderly patients. Identifying elderly patients who are at risk for developing chemotherapy related toxicity, remains an unmet need.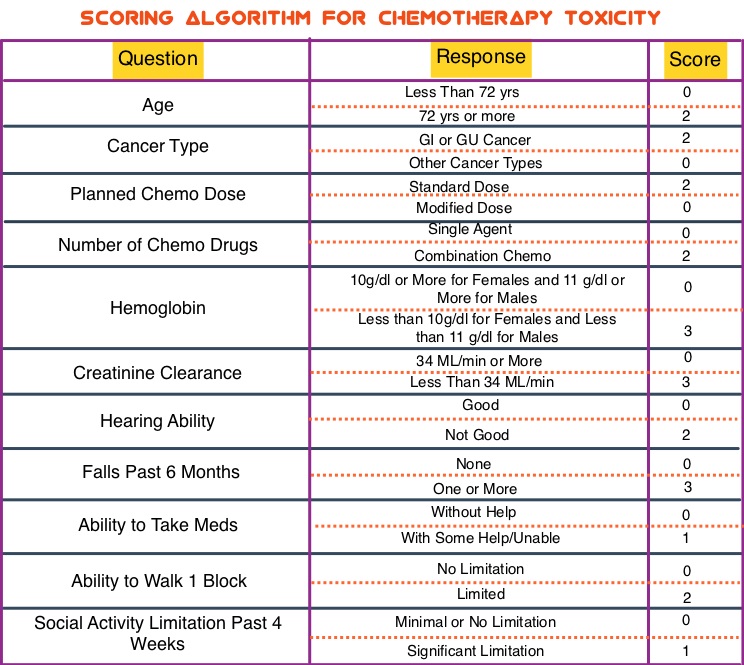
In this study, researchers developed a predictive model for chemotherapy toxicity, which consisted of 11 questions pertaining to age, tumor type, treatment, lab values and geriatric assessment, using data collected from a prospective longitudinal study of 500 patients, 65 years or older. Based on the answers to the 11 questions, a score for the risk of chemotherapy toxicity was calculated and three risk groups were created – Low (0-5 points), Medium (6-9 points) and High (10-19 points). In this Development cohort, the risk for chemotherapy toxicity correlated with an increasing risk score with 53% of patients experiencing grade 3 or higher chemotherapy toxicity.
The authors then validated the predictive model in an independent cohort of elderly adults (N=250) with a median age of 73 years. It was noted that more than one half of patients in the Validation cohort (58%) experienced grade 3 or more toxicity of whom 34% experienced hematologic toxicity and 55% experienced nonhematologic toxicity. The risk of toxicity increased with increasing risk score (36.7% for low risk cohort, 62.4% for medium risk cohort and 70.2% for high risk cohort; P<0.001). These findings were not statistically different from the Development cohort. Interestingly, there was no association between Karnofsky Performance Status and chemotherapy toxicity (P=0.25).
In elderly patients receiving chemotherapy, this tool is best used to distinguish low and high risk patients but is unable to distinguish moderate and high risk patients. Further, this model was only able to predict grade 3 or more toxicity but not grade 2 toxicity, and this may be equally relevant in elderly patients. Because patients included in this study had solid tumors and did not receive biologics or high-dose chemotherapy, these results apply primarily to patients with solid tumors who receive chemotherapy.
The authors concluded that this prediction model is easy to use in clinical practice and allows Oncology Health Care Providers to help elderly patients make informed decisions and also anticipate potential toxicities in high risk elderly patients and take preventive measures accordingly. Validation of a Prediction Tool for Chemotherapy Toxicity in Older Adults with Cancer. Hurria A, Mohile S, Gajra A, et al. J Clin Oncol 2016;34:2366-2371

