SUMMARY: The American Cancer Society estimates that for 2019 about 228,150 new cases of lung cancer will be diagnosed and 142,670 patients will die of the disease. Non Small Cell Lung Cancer (NSCLC) accounts for approximately 85% of all lung cancers. Patients with newly diagnosed metastatic NSCLC are often tested for guideline-recommended genomic biomarkers which include both predictive biomarker mutations such as EGFR, ALK, ROS1, BRAF, RET, MET, ERBB2, as well as prognostic biomarker mutation such as KRAS.
The application of precision medicine with targeted therapy requires detection of molecular abnormalities in a tissue biopsy specimen. However, if testing is not done with a comprehensive assay, such as Next-Generation Sequencing and is done in successive steps one test after another, tissue sample can be depleted, with not enough tissue left for testing of all biomarkers. Following progression or recurrence, archived biopsy specimens may not be helpful, as it is important to identify additional mutations in the tumor at the time of recurrence or progression, in order to plan appropriate therapy. Further, recurrent tumors may be inaccessible for a safe biopsy procedure or the clinical condition of the patient may not permit a repeat biopsy. Additionally, the biopsy itself may be subject to sampling error due to tumor heterogeneity. Genotyping circulating cell-free tumor DNA (cfDNA) in the plasma can potentially overcome the shortcomings of repeat biopsies and tissue genotyping, allowing the detection of many more targetable gene mutations, thus resulting in better evaluation of the tumor genome landscape.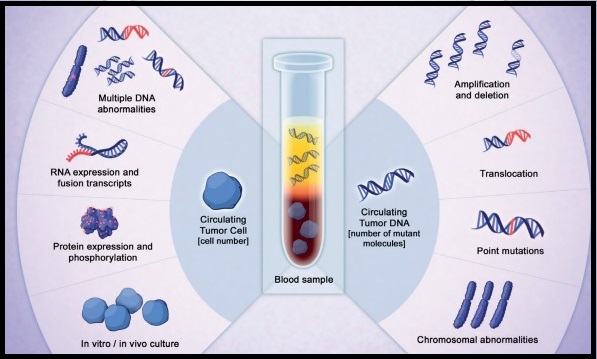
The Noninvasive versus Invasive Lung Evaluation (NILE) trial is a prospective, multicenter study conducted to demonstrate the noninferiority of comprehensive cell-free DNA (cfDNA) relative to standard-of-care traditional tissue genotyping tests, to identify guideline-recommended genomic biomarkers, in patients with metastatic NSCLC. The authors in this study enrolled 282 newly diagnosed patients at 28 North American centers, with previously untreated, nonsquamous, metastatic NSCLC undergoing standard-of-care tissue genotyping. Enrolled patients submitted a pretreatment blood sample for cfDNA analysis utilizing a CLIA-certified comprehensive 73-gene next generation sequencing panel (Guardant360®). Over 80% of the enrolled patients were white and over 50% were female.
The liquid biopsy utilizing Guardant360®, detected biomarker mutations at a rate similar to standard-of-care tissue genotyping tests, in the enrolled patients, meeting the Primary study objective. At least one of the guideline-recommended genomic biomarkers was detected in 60 patients (21.3%) using tissue-based tests and in 77 patients (27.3%) by cfDNA utilizing Guardant360® (P<0.0001). The detection rate was increased by 48% when Guardant360® was utilized for cfDNA analysis and this included those with negative, not assessed, or Quantity Not Sufficient (QNS) results in tissue. In addition, the Positive Predictive Value was 100% for cfDNA versus tissue genotyping, for FDA approved targets such as EGFR, ALK, ROS1, and BRAF mutations. There are agents already approved by the FDA to treat this patient population. The median turnaround time was significantly lower for cfDNA, compared to tissue genotyping (9 versus 15 days; P <0.0001).
The authors concluded that in this largest cfDNA study among patients with previously untreated advanced NSCLC, cfDNA successfully detected seven biomarker mutations noninvasively, significantly faster than tissue genotype testing, and was also able to rescue biomarker mutation positive patients who had non-diagnostic tissue results. They added that the findings in this study confirms similar findings from Europe and demonstrates the clinical utility of cfDNA in newly diagnosed metastatic NSCLC. Clinical utility of comprehensive cell-free DNA (cfDNA) analysis to identify genomic biomarkers in newly diagnosed metastatic non-small cell lung cancer (mNSCLC). Leighl N, Page RD, Raymond VM, et al. Presented at: AACR Annual Meeting April 2, 2019; Philadelphia, USA.

