SUMMARY: Lung cancer is the second most common cancer in both men and women and accounts for about 14% of all new cancers and 27% of all cancer deaths. The American Cancer Society estimates that for 2019, about 228,150 new cases of lung cancer will be diagnosed and 142,670 patients will die of the disease. Lung cancer is the leading cause of cancer-related mortality in the United States. Non-Small Cell Lung Cancer (NSCLC) accounts for approximately 85% of all lung cancers. Of the three main subtypes of NSCLC, 30% are Squamous Cell Carcinomas (SCC), 40% are Adenocarcinomas and 10% are Large Cell Carcinomas. With changes in the cigarette composition and decline in tobacco consumption over the past several decades, Adenocarcinoma now is the most frequent histologic subtype of lung cancer.
Approximately 10-15% of Caucasian patients and 35-50% of Asian patients with Adenocarcinomas, harbor activating EGFR (Epidermal Growth Factor Receptor) mutations and 90% of these mutations are either Exon 19 deletions or L858R substitution mutation in Exon 21. Approximately 25% of patients with EGFR mutated NSCLC have brain metastases at diagnosis, increasing to approximately 40% within two years of diagnosis. The presence of brain metastases often reduces median survival to less than eight months. EGFR-Tyrosine Kinase Inhibitors (TKIs) such as TARCEVA® (Erlotinib), IRESSA® (Gefitinib) and GILOTRIF® (Afatinib), have demonstrated a 60-70% response rate as monotherapy when administered as first line treatment, in patients with metastatic NSCLC, who harbor the sensitizing EGFR mutations. However, majority of these patients experience disease progression within 9-14 months. This resistance to frontline EGFR TKI therapy has been attributed to the most common, acquired T790M “gatekeeper” point mutation in EGFR, identified in 50-60% of patients.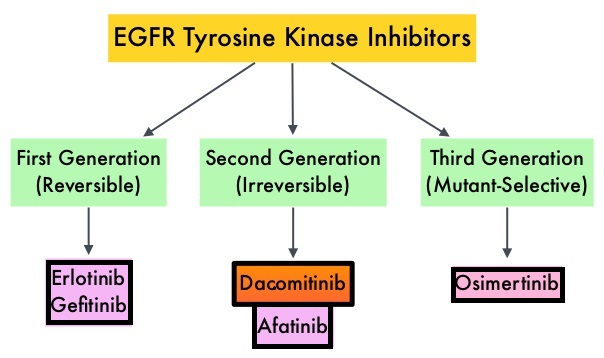
TAGRISSO® (Osimertinib) is a highly selective third-generation Epidermal Growth Factor Receptor (EGFR) TKI presently approved by the FDA, for the first-line treatment of patients with metastatic NSCLC, whose tumors have Exon 19 deletions or Exon 21 L858R mutations, as well as treatment of patients with metastatic EGFR T790M mutation-positive NSCLC, whose disease has progressed on or after EGFR-TKI therapy. Further, TAGRISSO® has higher CNS penetration and is therefore able to induce responses in 70-90% of patients with brain metastases.
FLAURA, which is a randomized, double blind, Phase III clinical trial, was conducted to compare the efficacy and safety of first line TAGRISSO® to TARCEVA® or IRESSA® (the latter two are considered standard first line therapies), in NSCLC patients with sensitizing EGFR mutations. This study randomized 556 advanced NSCLC treatment naïve patients, with EGFR Exon 19 Deletions or Exon 21 (L858R) substitution mutations, in a 1:1 ratio, to TAGRISSO® 80 mg orally once daily (N=279) or Standard of Care EGFR-TKI, IRESSA® 250 mg or TARCEVA® 150 mg, orally once daily (N=277). Patients were stratified by mutation status (Exon 19 vs 21 mutations) and race (Asian vs non-Asian). Patients with CNS metastases who were neurologically stable, were allowed in this study. The Primary endpoint was Progression Free Survival (PFS) and Overall Survival (OS) was a Secondary endpoint.
The median PFS was 18.9 months with TAGRISSO®, compared to 10.2 months for the standard therapy (HR=0.46; P<0.001), suggesting a 54% reduction in the risk of disease progression, compared with Standard of Care. TAGRISSO® extended the median Time To Progression by about 9 months. This PFS benefit was consistent across all subgroups of patients, including those with and without CNS metastases at study entry. The Objective Response Rate (ORR) with TAGRISSO® was 80% compared with 76% for TARCEVA® and IRESSA®. The median Duration of Response with TAGRISSO® was 17.2 months versus 8.5 months in the comparator arm.
The authors now reported the Overall Survival (OS) results from the Phase III FLAURA trial. Approximately, 25% of patients in the comparator group had crossed over to the TAGRISSO® group upon disease progression. Despite this crossover, the OS was significantly prolonged with TAGRISSO® with a median OS of 38.6 months compared with 31.8 months for the comparator arm (HR=0.799; P=0.046), representing a 20% reduction in the risk of death with TAGRISSO®. At the time of final data cutoff for the study, about 54% of patients remained alive at 3 years in the TAGRISSO® group compared with 44% in the comparator group, and 28% of patients enrolled in the trial were still receiving TAGRISSO® at three years versus 9% on either TARCEVA® or IRESSA®. Treatment with TAGRISSO® also resulted in a statistically significant and clinically meaningful 52% reduction in the risk of CNS disease progression or death, compared to the comparator arm (HR=0.48; P=0.014). Fewer patients in the TAGRISSO® group experienced Grade 3 or more Adverse Events compared to the comparator arm. Approximately 30% of patients in both treatment groups did not receive subsequent therapy after progression.
It was concluded that among patients with metastatic, EGFR-mutant NSCLC, first-line treatment with TAGRISSO®, significantly improved median Overall Survival, compared with TARCEVA® and IRESSA®, and should therefore be considered the preferred regimen. Osimertinib vs comparator EGFR-TKI as first-line treatment for EGFRm advanced NSCLC (FLAURA): Final overall survival analysis. Ramalingam SS, Gray JE, Ohe Y, et al. Presented at 2019 ESMO Congress, Barcelona, Spain, September 28 to October 1, 2019. Abstract LBA5_PR.

