SUMMARY: The American Cancer Society estimates that in 2016, about 72,580 people will be diagnosed with Non Hodgkin Lymphoma (NHL) in the United States and about 20,150 individuals will die of this disease. Patients with refractory DLBCL have poor outcomes with chemotherapy, and have a response rate of 20%-30% and median overall survival of approximately 6 months (J Clin Oncol 34, 2016, suppl; abstr. 7516), and thus represents a significant unmet medical need. Chimeric Antigen Receptor (CAR) T-cell therapy is a type of immunotherapy in which T cells are collected from the patient’s own blood and are genetically engineered to produce special receptors on their surface called Chimeric Antigen Receptors (CAR’s). The cytotoxic T cells with these chimeric antigen receptors on their surface are now able to recognize a specific antigen on tumor cells. These engineered CAR T-cells which are grown in the lab are then infused into the patient and they in turn proliferate in the patient’s body and the engineered receptor on their surface help recognize and kill cancer cells that expresses that specific antigen. CD19 antigen is expressed by majority of the B cell malignancies and therefore most studies using CAR T-cell therapy have focused on the treatment of advanced B-cell malignancies such as Chronic Lymphocytic Leukemia (CLL), Acute Lymphoblastic Leukemia (ALL) and Non Hodgkin lymphoma (NHL), such as Diffuse Large B-Cell Lymphoma (DLBCL).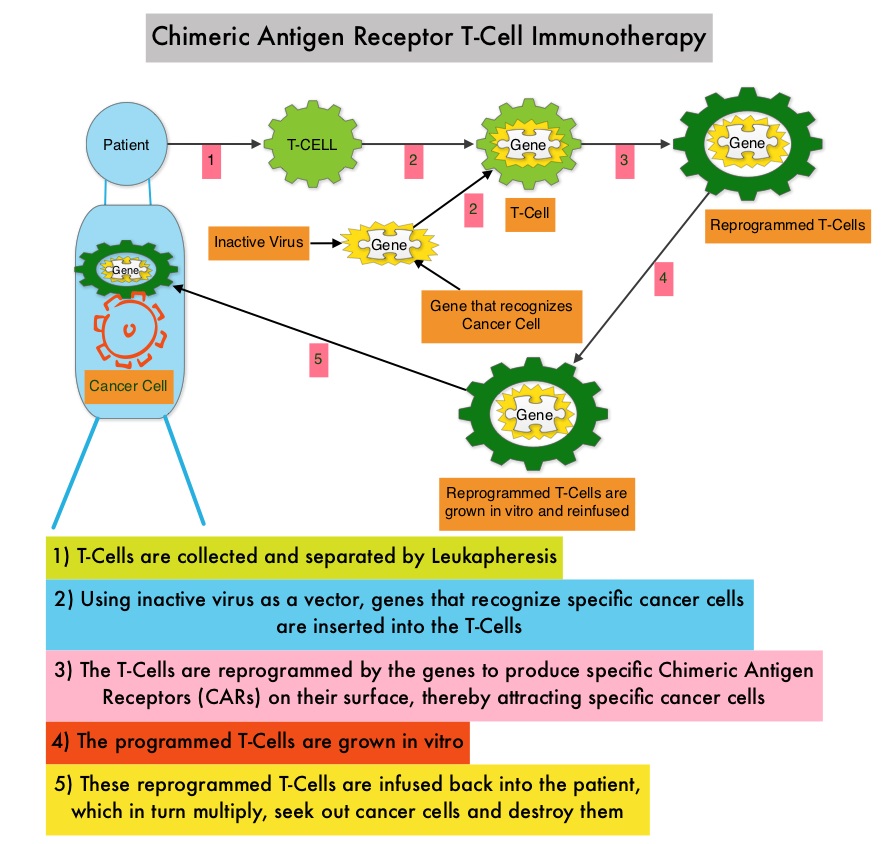
The KTE-C19 (anti-CD19 Chimeric Antigen Receptor (CAR) T cells) construct consists of an extracellular domain which recognizes and targets the CD19 antigen on the surface of tumor cells, and the intracellular domains to avoid activation of hidden signals to the T-cells. ZUMA-1 is a multicenter phase I/II trial of anti-CD19 Chimeric Antigen Receptor (CAR) T cells (KTE-C19) in refractory, aggressive NHL and this study included patients with Diffuse Large B-Cell Lymphoma (DLBCL), Primary Mediastinal B-Cell Lymphoma (PMBCL), and Transformed Follicular Lymphoma (TFL). In the phase I component of this study, 43% of the patients had ongoing Complete Responses at 12 months.
Phase II of ZUMA-1 included 2 patient cohorts based on the tumor type. Cohort 1 included DLBCL and patients in cohort 2 had PMBCL or TFL. Refractory disease was defined as progressive or stable disease as best response to last line of therapy, or disease progression 12 months or less after Autologous Stem Cell Transplant (ASCT). All included patients received a prior anti-CD20 antibody and an Anthracycline-containing regimen. The median age was 58 years, 78% were refractory to 2 or more lines of therapy, 20% relapsed less than 12 months after ASCT. Patients received a low-dose conditioning regimen of Cyclophosphamide 500 mg/m2 IV and Fludarabine 30 mg/m2 IV, daily for 3 days followed by a target dose of 2 × 106 anti-CD19 CAR T cells/kg. The primary endpoint was Objective Response Rate (ORR) and secondary endpoints include Duration of Response, frequency of adverse events (AEs), and levels of CAR T cells and serum cytokines. The authors presented the results of a pre-specified interim analysis from cohort 1 and 51 patients in cohort 1 were eligible for analysis.
The study met its primary endpoint and with a minimal follow up of three months, the ORR was 76% compared with ORR of 20% in historical controls (P<0.0001). Complete Responses were noted in 47% of the patients and Partial Response rate was 29%. Majority of the responses (92%) occurred within the first month, and the Complete Response Rate at 3 months was 33% and 39% of the patients had ongoing responses at 3 months. The treatment benefit was consistent across all subgroups of patients. The most frequent more than grade 3 toxicities were cytopenias, encephalopathy and hypophosphatemia. Grade 3 or more Cytokine Release Syndrome (CRS) and neurologic events occurred in 20-30% of the patients.
The authors concluded that this is the first reported multicenter trial of CAR T cell therapy in patients with refractory aggressive NHL and therapy with KTE-C19 induced a nearly six fold higher Complete Response Rate compared to historical outcomes and efficacy was strongly associated with peak CAR T levels. KTE-C19 (anti-CD19 CAR T Cells) Induces Complete Remissions in Patients with Refractory Diffuse Large B-Cell Lymphoma (DLBCL): Results from the Pivotal Phase 2 ZUMA-1.Neelapu SS, Locke FL, Bartlett NL, et al. Presented at: American Society of Hematology 58th Annual Meeting; December 3-6, 2016; San Diego, CA. Abstract LBA6.

