SUMMARY: The FDA on May 8, 2020, granted accelerated approval to RETEVMO® (Selpercatinib) for patients with metastatic RET fusion-positive Non-Small Cell Lung Cancer (NSCLC), patients with advanced or metastatic RET-mutant Medullary Thyroid Cancer (MTC) who require systemic therapy and those with advanced or metastatic RET fusion-positive thyroid cancer who require systemic therapy and who are RadioActive Iodine (RAI)-refractory. Lung cancer is the second most common cancer in both men and women and accounts for about 14% of all new cancers and 27% of all cancer deaths. The American Cancer Society estimates that for 2020, about 228, 820 new cases of lung cancer will be diagnosed and 135,720 patients will die of the disease. Lung cancer is the leading cause of cancer-related mortality in the United States. Non-Small Cell Lung Cancer (NSCLC) accounts for approximately 85% of all lung cancers.
In addition to the well characterized gene fusions involving ALK and ROS1 in NSCLC, genetic alterations involving other kinases including EGFR, BRAF, RET, NTRK, are all additional established targetable drivers. These genetic alterations are generally mutually exclusive, with no more than one predominant driver in any given cancer. The hallmark of all of these genetic alterations is oncogene addiction, in which cancers are driven primarily, or even exclusively, by aberrant oncogene signaling, and are highly susceptible to small molecule inhibitors.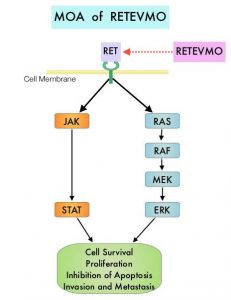
RET kinase is a transmembrane Receptor Tyrosine Kinase and plays an important role during the development and maintenance of a variety of tissues, including neural and genitourinary tissues. RET signaling activates downstream pathways such as JAK/STAT3 and RAS/RAF/MEK/ERK and leads to cellular proliferation, survival, invasion, and metastasis. Oncogenic alterations to the RET proto-oncogene results in uncontrolled cell growth and enhanced tumor invasiveness. RET alterations include RET rearrangements, leading to RET fusions, and activating point mutations occurring across multiple tumor types. RET fusions have been identified in approximately 2% of NSCLCs, 10-20% of non-medullary thyroid cancers. Activating RET point mutations account for approximately 60% of sporadic Medullary Thyroid Cancers (MTC) and more than 90% of inherited MTCs. Other cancers with documented RET alterations include colorectal, breast, and several hematologic malignancies.
RETEVMO® (Selpercatinib) is a highly selective and potent, oral anti-RET Tyrosine Kinase Inhibitor (TKI) designed to inhibit native RET signaling, as well as anticipated acquired resistance mechanisms. RETEVMO® selectively targets wild-type RET as well as various RET mutants and RET-containing fusion products. Additionally, RETEVMO® inhibits Vascular Endothelial Growth Factor Receptor 1 (VEGFR1), VEGFR3, Fibroblast Growth Factor Receptor 1 (FGFR1), FGFR2, and FGFR3. This results in inhibition of cell growth of tumors that exhibit increased RET activity.
The LIBRETTO-001 is the largest open-label, multicenter, Phase I/II trial in patients with advanced solid tumors, including RET fusion-positive solid tumors, RET-mutant Medullary Thyroid Cancers, and other tumors with RET activation, treated with a RET inhibitor. To investigate the efficacy of RETEVMO®, the trial was conducted in 2 parts: Phase 1 (dose escalation) and Phase II (dose expansion). Patients with advanced cancer were eligible, if they have progressed on or were intolerant to available standard therapies, or no standard or available curative therapy existed, or in the opinion of the Investigator, they would be unlikely to tolerate or derive significant clinical benefit from appropriate standard of care therapy, or they declined standard therapy. A dose of 160 mg BID was the recommended Phase II dose. Up to about 850 patients with advanced solid tumors harboring a RET gene alteration in tumor and/or blood were enrolled in 6 different Phase II cohorts, based on tumor type, RET alteration and prior therapy. Identification of RET gene alterations was prospectively determined in local laboratories using either Next Generation Sequencing, Polymerase Chain Reaction, or Fluorescence In Situ Hybridization. The Phase II portion of the trial had a Primary endpoint of Objective Response Rate (ORR) and Secondary endpoints of Duration of Response, Progression Free Survival (PFS) and safety.
The NSCLC cohort included 105 enrolled patients with RET fusion-positive NSCLC who had received prior platinum-based chemotherapy. Patients had received a median of three prior systemic regimens, 55% had previous treatment with an anti-PD-1/PD-L1 antibody and 48% had previous treatment with at least one multikinase inhibitor. The ORR with RETEVMO® was 64%, and 81% of responding patients had responses lasting 6 months or longer. Efficacy was also evaluated in 39 treatment-naïve patients. The ORR for these patients with RETEVMO® was 85%, and 58% of responding patients had responses lasting 6 months or longer. It is estimated that up to 50% of RET fusion-positive NSCLC patients can have brain metastases, and in the subset of patients with brain metastases in this registrational trial, treatment with RETEVMO® demonstrated a CNS Objective Response Rate of 91%. Median DOR and PFS were not reached at the time of data-cut-off.
In the cohort of advanced or metastatic RET-mutant MTC (N=143), the ORR in patients previously treated with COMETRIQ® (Cabozantinib), CAPRELSA® (Vandetanib), or both (N=55) was 69%, and 76% of responding patients had responses lasting 6 months or longer. Among those patients who had no prior therapy with an approved agent for MTC (N=88), the ORR was 73%, and 61% of responding patients had responses lasting 6 months or longer.
In the cohort of RET fusion-positive thyroid cancer who were RAI-refractory and had received another prior systemic treatment (N=19), the ORR was 79%, and 87% of responders had a response lasting 6 months or longer. Among the patients with RET fusion-positive thyroid cancer who were RAI-refractory and had not received any additional therapy (N=8), the ORR was 100% and 75% of responders had a response lasting 6 months or longer.The most common toxicities included rash, cytopenias, liver function abnormalities, hyperglycemia, hyponatremia, hypocalcemia, increased creatinine and hypertension.
LIBRETTO-001 is the largest trial ever reported in RET-altered cancer patients, and the present FDA approval of RETEVMO® for patients with RET fusions and mutations, across multiple tumor types, represents an important milestone in the Precision Medicine arena.
https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-selpercatinib-lung-and-thyroid-cancers-ret-gene-mutations-or-fusions

