SUMMARY: The Center for Disease Control and Prevention (CDC) estimates that approximately 1-2 per 1000 individuals develop Deep Vein Thrombosis/Pulmonary Embolism (PE) each year in the United States, resulting in 60,000-100,000 deaths. Venous ThromboEmbolism (VTE) is the third leading cause of cardiovascular mortality. Patients with unprovoked DVT and PE are two to four times more likely to be diagnosed with cancer within the ensuing 12 months compared to the general population. Approximately 20% of VTE events are related to underlying malignancy and patients with active malignancy have a five to six fold increased risk of VTE. In patients with cancer associated thrombosis, COUMADIN® (Warfarin) and XARELTO® (Rivaroxaban) are often prescribed, despite guidelines recommending Low Molecular Weight Heparin (LMWH) in this patient population. However, patients are less inclined to take LMWH as this is parenteral, expensive, inconvenient and carries the risk of Heparin-Induced Thrombocytopenia. Further, most patients with malignancy require indefinite anticoagulation and the safety and efficacy of LMWH in this setting is unknown. The efficacy and safety of oral, direct Factor Xa inhibitor such as XARELTO® is not well established in patients with VTE and active malignancy.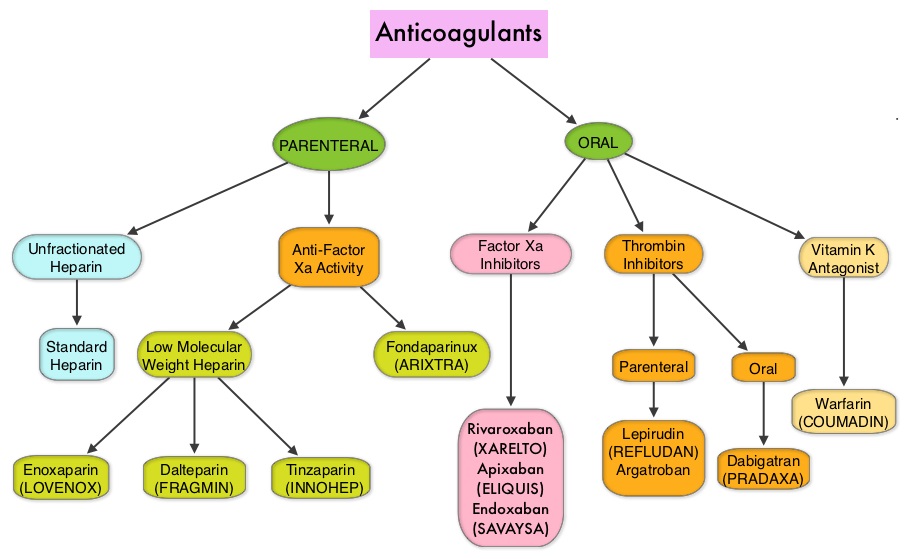
The authors in this study evaluated the risk and benefits of XARELTO® in this high-risk group of patients. In this case cohort study, the Mayo Thrombophilia Clinic Direct Oral Anticoagulants Registry included patients diagnosed with Deep Vein Thrombosis or Pulmonary Embolism, who were seen and treated with XARELTO® at the Thrombophilia Clinic, Gonda Vascular Center and Mayo Clinic in Rochester, Minn. These units work together and provide streamlined standardized care. Immediate anticoagulation therapy was provided for appropriate patients. Patients with symptomatic PE or extensive symptomatic iliofemoral Deep Vein Thrombosis were hospitalized. All patients with PE also had lower extremity duplex ultrasound to determine the source of embolism. Evaluation included upper extremity venous assessment, if a patient had symptoms suggestive of venous thrombosis or if a Central Venous Catheter was present.
Patients with acute VTE or asymptomatic PE suitable for outpatient anticoagulation therapy were counseled about the pros and cons of each anticoagulant currently approved by the FDA. Additionally, patients with active malignancy and VTE were counseled about the preferred first line of treatment with Low Molecular Weight Heparin, as well as the limited data for XARELTO® in cancer-associated VTE. Patients opting for XARELTO®, were started on treatment within the ensuing hour. Patients were evaluated every 3 months for efficacy and safety and followed prospectively from March 2013 and April 2015. The primary efficacy outcome was symptomatic venous or arterial thromboembolism occurring during the follow up period. The primary safety end point was major bleeding defined as overt bleeding plus a hemoglobin decrease of 2 or more grams/dL after the incident, transfusion of 2 or more units of packed red blood cells, or intracranial, intraspinal, intraocular, retroperitoneal, pericardial, or fatal bleeding.
Two hundred and ninety six (N=296) of the 404 patients in the registry with Venous ThromboEmbolism (VTE), received XARELTO® and had at least 3 months of follow up. Of these 296 patients on XARELTO®, 118 patients (40%) had active malignancy and 178 patients had no cancer. The 3 most common cancer locations were Genitourinary (23.6%), Gastrointestinal (20.3%) and Lung (13.5%). It was noted that there was no significant difference in VTE recurrence between the malignant (3.3%) and the nonmalignant (2.8%) VTE groups (P=0.533). Slightly higher rates for major bleeding (P=0.06) and non major clinically relevant bleeding (P=0.08) were noted in patients with cancer, but this was not statistically significant.
The authors concluded that the efficacy and safety of XARELTO® is similar for VTE patients with and without active malignancy. Efficacy and Safety of Rivaroxaban in Patients with Venous Thromboembolism and Active Malignancy: A Single-Center Registry. Bott-Kitslaar DM, Saadiq RA, McBane RD, et al. Am J Med. 2016; 129: 615-619

