SUMMARY: Lung cancer is the second most common cancer in both men and women and accounts for about 14% of all new cancers. The American Cancer Society estimates that for 2018 about 234,030 new cases of lung cancer will be diagnosed and over 154,050 patients will die of the disease. Non Small Cell Lung Cancer (NSCLC) accounts for approximately 85% of all lung cancers. Of the three main subtypes of Non Small Cell Lung Cancer (NSCLC), 30% are Squamous Cell Carcinomas (SCC), 40% are Adenocarcinomas and 10% are Large cell carcinomas. Immunotherapy is an accepted second line intervention after platinum-based chemotherapy in patients with advanced NSCLC, and is an approved first line therapy, for patients with high PD-L1 expressing tumors (50% or more). Further, immunotherapy with KEYTRUDA® (Pembrolizumab), in combination with chemotherapy, has been approved for first line treatment of patients with advanced non-squamous NSCLC, irrespective of PD-L1 expression.
TECENTRIQ® (Atezolizumab) is an anti-PDL1 monoclonal antibody, designed to directly bind to PD-L1 expressed on tumor cells and tumor-infiltrating immune cells, thereby blocking its interactions with PD-1 and B7.1 receptors and thus enabling the activation of T cells. TECENTRIQ® was approved by the FDA in October 2016 for the treatment of patients with metastatic Non Small Cell Lung Cancer (NSCLC) whose disease progressed during or following Platinum-containing chemotherapy. AVASTIN® (Bevacizumab) is a biologic antiangiogenic antibody, directed against Vascular Endothelial Growth Factor (VEGF), and prevents the interaction of VEGF to its receptors (Flt-1 and KDR) on the surface of endothelial cells. The interaction of VEGF with its receptors has been shown to result in endothelial cell proliferation and new blood vessel formation. Combining TECENTRIQ® and AVASTIN® is supported by the following scientific rationale. AVASTIN® in addition to its established anti-angiogenic effects, may further enhance the ability of TECENTRIQ® to restore anti-cancer immunity, by inhibiting VEGF-related immunosuppression, promoting T-cell tumor infiltration and enabling priming and activation of T-cell responses against tumor antigens.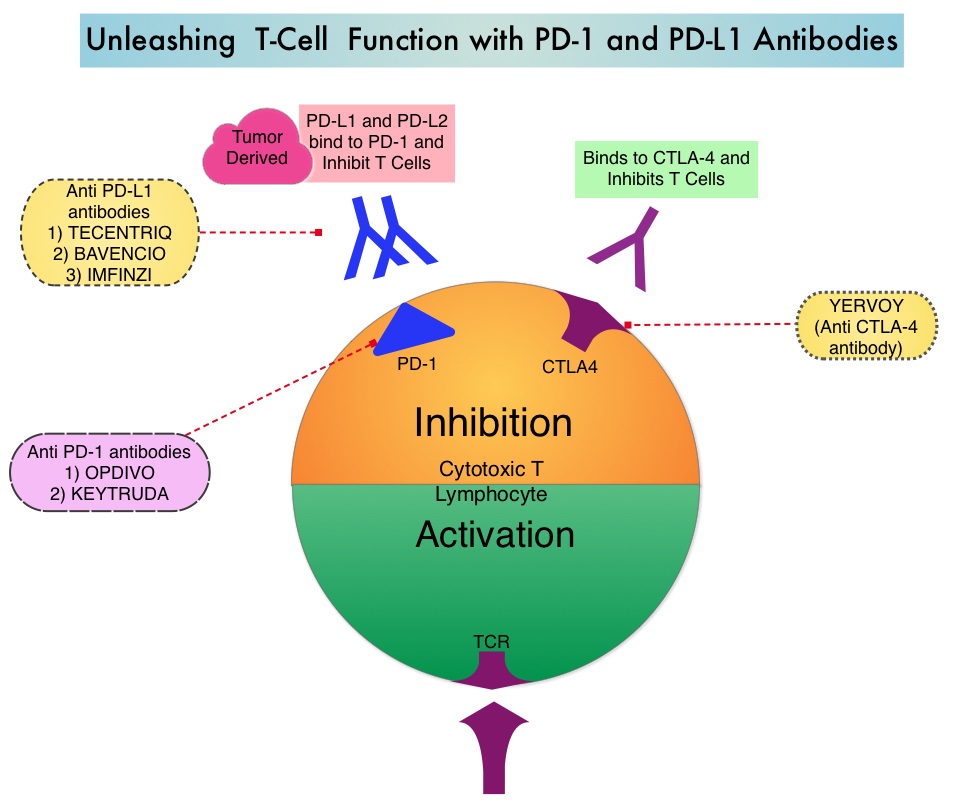
IMpower150 is a multicenter, open-label, randomized, phase III study, conducted to evaluate the efficacy and safety of TECENTRIQ® in combination with Carboplatin and Paclitaxel with or without AVASTIN®, in patients with stage IV, treatment naïve, non-squamous NSCLC. This study enrolled 1,202 patients, who were randomized (1:1:1) to receive either TECENTRIQ® along with Carboplatin and Paclitaxel (Group A), TECENTRIQ® and AVASTIN® along with Carboplatin and Paclitaxel (Group B), or AVASTIN® plus Carboplatin and Paclitaxel (Group C – control arm). During the treatment-induction phase, patients in Group A received TECENTRIQ® 1200 mg IV along with Carboplatin AUC 6 and Paclitaxel 200mg/m2 IV on Day 1 of a 3-week treatment cycle for 4 or 6 cycles. Following the induction phase, patients received maintenance treatment with TECENTRIQ® on the same dose schedule until disease progression. Patients in Group B received AVASTIN® 15 mg/kg IV, along with TECENTRIQ®, Carboplatin and Paclitaxel IV, Day 1 of a 3-week treatment cycle for 4 or 6 cycles followed by maintenance treatment with the TECENTRIQ® and AVASTIN® until disease progression. Patients in the control Group C received AVASTIN® plus Carboplatin and Paclitaxel every 3 weeks for 4 or 6 cycles followed by AVASTIN® maintenance treatment until disease progression. Patients with tumors demonstrating ALK and EGFR mutations were excluded from the primary Intention-To-Treat (ITT) analysis. Patients were also tested for a tumor T-effector gene expression signature (based on phase II trial finding of prolonged Overall Survival in patients with high gene expression signature levels, treated with TECENTRIQ®). The median age was 63 years and the minimum follow up at the time of the analysis was 9.5 months. For the interim analysis, the study was only designed to compare Groups B and C. The co-Primary endpoints were Progression Free Survival (PFS) and Overall Survival in the Intention-to-Treat (ITT) population comparing patients in Group B and C. These end points were also evaluated in subgroup of people who had a specific biomarker (T-effector gene signature expression).
It was noted that at this interim analysis, the combination of TECENTRIQ® and AVASTIN® plus Carboplatin and Paclitaxel, significantly improved PFS and reduced the risk of disease worsening or death by 38% (HR=0.62; P<0.0001), compared to AVASTIN® plus Carboplatin and Paclitaxel alone. This PFS benefit was observed across key subgroups, regardless of PD-L1 expression status, including PD-L1–negative patients (HR 0.77). Further, the median PFS in the population of patients with defined expression of a T-effector gene signature expression in the tumor tissue, was 11.3 months versus 6.8 months (HR 0.51; P<0.0001). Roche on March 26, 2018 announced that the IMpower150 study met its co-primary endpoint of Overall Survival as well. Details will soon become available.
It was concluded that combining chemotherapy with immunotherapy and antiangiogenic agents significantly improved PFS as well as Overall Survival, in patients with treatment naïve, advanced non-squamous NSCLC. This strategy can completely eliminate the need for patient selection based on a particular biomarker, and could benefit larger number of patients with advanced NSCLC. Reck M. Primary PFS and safety analyses of a randomized Phase III study of carboplatin + paclitaxel +/− bevacizumab, with or without atezolizumab in 1L non-squamous metastatic NSCLC (IMpower150). Annals of Oncology, 2017;28(11). Abstract LBA1_PR. https://www.roche.com/media/store/releases/med-cor-2018-03-26.htm

