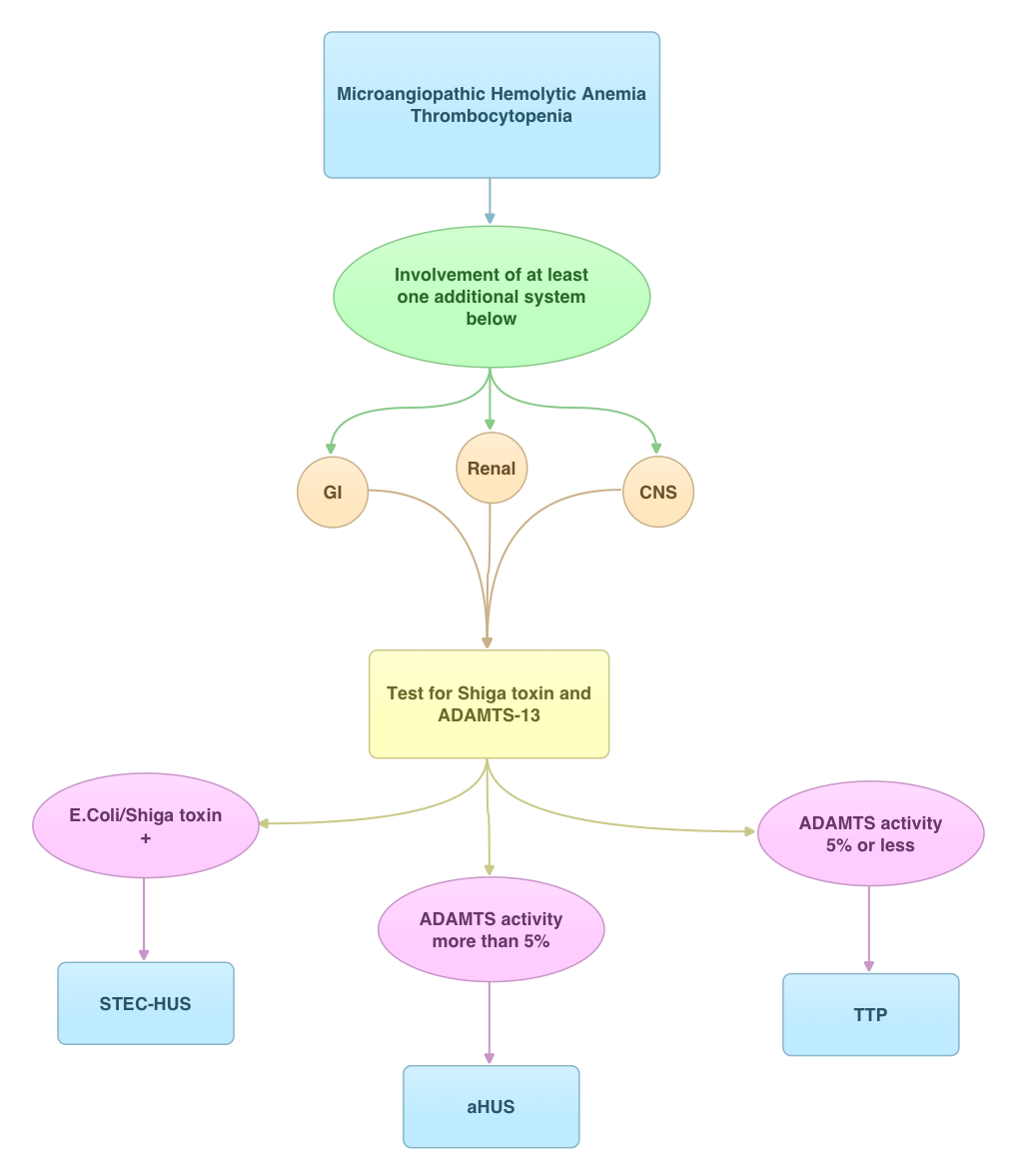
SUMMARY: Thrombotic Thrombocytopenic Purpura (TTP), Hemolytic Uremic Syndrome (HUS) and Atypical Hemolytic Uremic Syndrome (aHUS) are Thrombotic Microangiopathies (TMA’s) associated with MicroAngiopathic Hemolytic Anemia and thrombocytopenia. Even though their clinical presentation has some similarities, they are distinct entities with different pathophysiology and hence managed differently. With the identification of von Willebrand Factor (vWF) cleaving protease ADAMTS13 (A disintegrin and metalloprotease with thrombospondin type 1 repeats, member 13) in 1996, we are now able to better understand and appropriately manage these TMA’s. Patients with TTP are deficient in ADAMTS13 and therefore develop platelet microthrombin in small blood vessels due to uninhibited propagation of platelet aggregates bound to ultra high molecular weight VWF multimers. Approximately 10% or less of Shiga-Toxin producing Escherichia Coli (STEC) infections may be associated with HUS. aHUS is caused by a genetic deficiency of one or more complement regulatory proteins which results in uncontrolled activity of the alternate complement pathway. Plasma Exchange in TTP restores the protease activity of ADAMTS13 whereas aHUS is treated with SOLIRIS® (Eculizumab) to inhibit complement mediated TMA. Once a diagnosis of STEC-HUS is confirmed, hospitalization and intensive care with transfusions and kidney dialysis may become necessary. George JN. Blood 2010:116; 4060-4069