SUMMARY: Squamous Cell Carcinoma of the Head and Neck (HNSCC) accounts for about 3-5% of all cancers in the United States. It is estimated that 55,070 people were diagnosed with Head and Neck cancer in 2014 and 12,000 patients died of the disease. The head and neck region includes the oral cavity, oropharynx, hypopharynx and larynx. Squamous Cell Carcinoma involving the head and neck region (HNSCC) is therefore a heterogeneous disease and the five year survival rate of patients with head and neck cancer depends on several factors and can be variable. Common risk factors include tobacco and alcohol use and Human PapillomaVirus (HPV) infection. Recent studies have shown that over 70% of the OroPharyngeal Squamous Cell Carcinomas (OPSCC) are caused by HPV with the HPV-16 being the predominant type present in the tumor cells.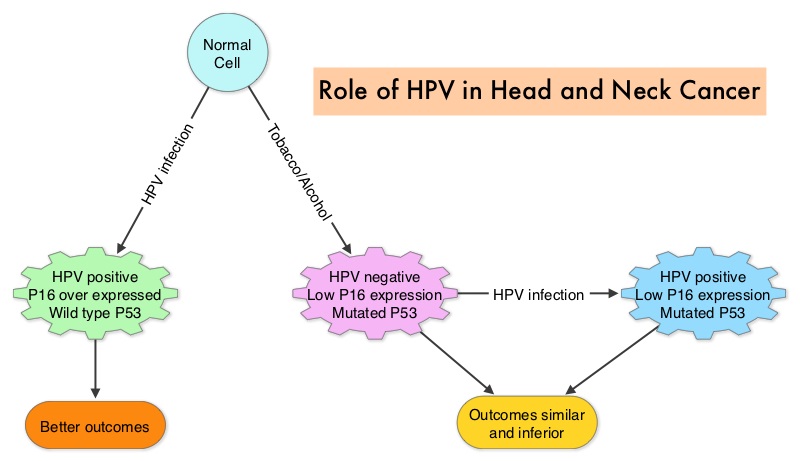 The malignant behavior of these tumors is dependent on the expression of viral E6 and E7 oncoproteins that inactivate the tumor suppressor proteins p53 and the retinoblastoma protein (pRB), respectively. HPV positive OroPharyngeal Squamous Cell Carcinoma (OPSCC) is more common among never smokers or light smokers and patients tend to be younger with better performance status. The pathobiology of HPV positive OroPharyngeal Squamous Cell Carcinoma (OPSCC) is different from the HPV negative OroPharyngeal Squamous Cell Carcinoma in that p53 is degraded/inactivated by viral E6 oncoprotein instead of by genetic mutation, pRB pathway is inactivated by viral E7 oncoprotein instead of Cyclin D1 amplification and p16 is overexpressed or upregulated instead of inactivation resulting from reduced negative feedback from pRB. Testing for HPV is based on several methodologies which include detection of HPV DNA by in situ hybridization (ISH) or Polymerase Chain Reaction (PCR), detection of HPV E6/E7 RNA expression by quantitative Reverse Transcriptase–PCR (qRT-PCR) and p16 protein overexpression, a surrogate marker of oncogenic HPV infection, by ImmunoHistoChemistry (IHC) staining. Both p16 overexpression testing by IHC and HPV by ISH can be easily performed on Formalin-Fixed Paraffin Embedded (FFPE) specimen whereas detection of HPV E6/E7 RNA expression, which is indicative of active viral oncogene transcription in tumor cells and is considered to be a gold standard, requires a larger tumor specimen compared with other methodologies.
The malignant behavior of these tumors is dependent on the expression of viral E6 and E7 oncoproteins that inactivate the tumor suppressor proteins p53 and the retinoblastoma protein (pRB), respectively. HPV positive OroPharyngeal Squamous Cell Carcinoma (OPSCC) is more common among never smokers or light smokers and patients tend to be younger with better performance status. The pathobiology of HPV positive OroPharyngeal Squamous Cell Carcinoma (OPSCC) is different from the HPV negative OroPharyngeal Squamous Cell Carcinoma in that p53 is degraded/inactivated by viral E6 oncoprotein instead of by genetic mutation, pRB pathway is inactivated by viral E7 oncoprotein instead of Cyclin D1 amplification and p16 is overexpressed or upregulated instead of inactivation resulting from reduced negative feedback from pRB. Testing for HPV is based on several methodologies which include detection of HPV DNA by in situ hybridization (ISH) or Polymerase Chain Reaction (PCR), detection of HPV E6/E7 RNA expression by quantitative Reverse Transcriptase–PCR (qRT-PCR) and p16 protein overexpression, a surrogate marker of oncogenic HPV infection, by ImmunoHistoChemistry (IHC) staining. Both p16 overexpression testing by IHC and HPV by ISH can be easily performed on Formalin-Fixed Paraffin Embedded (FFPE) specimen whereas detection of HPV E6/E7 RNA expression, which is indicative of active viral oncogene transcription in tumor cells and is considered to be a gold standard, requires a larger tumor specimen compared with other methodologies.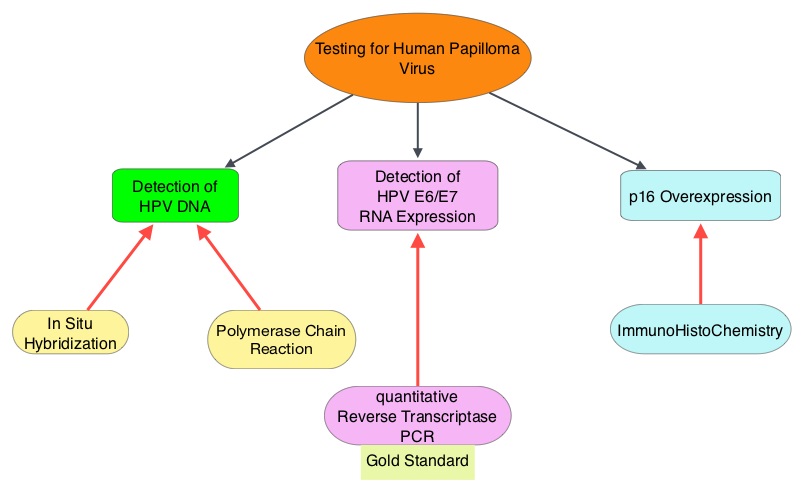 The concordance rate between HPV by ISH and p16 by IHC is approximately 90% in OPSCC, whereas the prevalence and significance p16 by IHC has remained unclear for HPV infection in non-OPSCC (oral cavity, hypopharynx and larynx). It is well established however that patients with HPV-positive/p16-positive OPSCC have better outcomes compared with those with HPV-negative/p16-negative OPSCC. However, the prognostic significance of p16 overexpression in non-OPSCC patients with or without evidence of HPV infection has not been clear. The authors in this study evaluated p16 protein overexpression by IHC and HPV status by HPV ISH as potential prognostic biomarkers in non-OPSCC tumors of patients enrolled in three prospective Radiation Therapy Oncology Group (RTOG) clinical trials. Of the 1921 patient enrolled in these three trials, 683 patients with non-OPSCC tumors were eligible and 52% (N=356) of these patients were tested for p16 overexpression and overall, 19.3% were p16 positive. When OPSCC and non-OPSCC patients were compared, OPSCC patients whose tumors were p16 positive had better Progression Free Survival and Overall Survival than non-OPSCC patients with p16 positive tumors. However, patients with p16 negative OPSCC and non-OPSCC have similar inferior outcomes. The authors concluded that patients with p16 negative non-OPSCC have worse outcomes than patients with p16 positive non-OPSCC, similar to that seen in patients with OPSCC and therefore HPV infection may influence outcomes in a subset of patients with non-OPSCC as well. Better methodologies for HPV detection and correlation with p16 expression will help identify “true” HPV infection related non-OPSCC and thereby enable tailored and less intense treatment, for this favorable group of patients. Chung CH, Zhang Q, Kong CS, et al. J Clin Oncol 2014; 32:3930-3938
The concordance rate between HPV by ISH and p16 by IHC is approximately 90% in OPSCC, whereas the prevalence and significance p16 by IHC has remained unclear for HPV infection in non-OPSCC (oral cavity, hypopharynx and larynx). It is well established however that patients with HPV-positive/p16-positive OPSCC have better outcomes compared with those with HPV-negative/p16-negative OPSCC. However, the prognostic significance of p16 overexpression in non-OPSCC patients with or without evidence of HPV infection has not been clear. The authors in this study evaluated p16 protein overexpression by IHC and HPV status by HPV ISH as potential prognostic biomarkers in non-OPSCC tumors of patients enrolled in three prospective Radiation Therapy Oncology Group (RTOG) clinical trials. Of the 1921 patient enrolled in these three trials, 683 patients with non-OPSCC tumors were eligible and 52% (N=356) of these patients were tested for p16 overexpression and overall, 19.3% were p16 positive. When OPSCC and non-OPSCC patients were compared, OPSCC patients whose tumors were p16 positive had better Progression Free Survival and Overall Survival than non-OPSCC patients with p16 positive tumors. However, patients with p16 negative OPSCC and non-OPSCC have similar inferior outcomes. The authors concluded that patients with p16 negative non-OPSCC have worse outcomes than patients with p16 positive non-OPSCC, similar to that seen in patients with OPSCC and therefore HPV infection may influence outcomes in a subset of patients with non-OPSCC as well. Better methodologies for HPV detection and correlation with p16 expression will help identify “true” HPV infection related non-OPSCC and thereby enable tailored and less intense treatment, for this favorable group of patients. Chung CH, Zhang Q, Kong CS, et al. J Clin Oncol 2014; 32:3930-3938
