The FDA on January 18, 2019 granted approval to ONTRUZANT®, a Trastuzumab (HERCEPTIN®) biosimilar, for the treatment of patients with HER2-overexpressing Breast cancer or metastatic Gastric or GastroEsophageal Junction adenocarcinoma. The newly approved biosimilar will also eventually compete with 2 prior FDA approved biosimilars, OGIVRI® (Trastuzumab-dkst) and HERZUMA® (Trastuzumab-pkrb). ONTRUZANT® is a product of Samsung Bioepis and will be marketed by Merck&Co.
Tag: Gastric and GE Junction Cancer
Adjuvant Chemotherapy May Improve Overall Survival Following Preoperative Chemoradiotherapy and Surgery in GastroEsophageal Cancer
SUMMARY: The American Cancer Society estimates that in the US, about 17,290 new Esophageal cancer cases will be diagnosed in 2018 and about 15,850 patients will die of the disease. Squamous Cell Carcinoma is the most common type of cancer of the Esophagus among African Americans, while Adenocarcinoma is more common in caucasians. Esophageal cancer is more common among men than among women. It is estimated that about 20% of patients survive at least 5 years after diagnosis.
Patients with resectable, locally advanced, Esophageal or GastricEsophageal junctional cancer are often treated with multimodality therapy. The CROSS trial (ChemoRadiotherapy for Oesophageal cancer followed by Surgery Study) compared neoadjuvant chemoradiotherapy with weekly Carboplatin and Paclitaxel plus Radiotherapy followed by surgery, to surgery alone, in patients with Squamous Cell Carcinoma and Adenocarcinoma of the Esophagus or GastricEsophageal junction. Neoadjuvant chemoradiotherapy when added to surgery in this study, conferred Overall Survival benefit, for both Squamous Cell Carcinoma and Adenocarcinoma histological subtypes and is now regarded as the standard of care, for this patient population. Nonetheless, it should be noted that the survival benefit was most pronounced in patients with squamous cell histology but was less definitive for those with adenocarcinoma histology, with approximately a third of patients developing distant failure. It has been postulated that the reduced dose and duration systemic chemotherapy given concurrently with radiation therapy, in preoperative setting, may have limited the efficacy of chemotherapy to prevent distant failure.
There is limited data on the role of adjuvant chemotherapy added to preoperative chemoradiotherapy and surgery, for patients with GastricEsophageal (GE) junctional adenocarcinoma. To address this question, the authors in this publication compared Overall Survival among patients with GE adenocarcinoma, receiving adjuvant chemotherapy versus postoperative observation, following preoperative chemoradiotherapy and surgical resection.
Using the National Cancer Database, the authors identified 10,086 patients, 9272 in the postoperative observation group and 814 who had received adjuvant chemotherapy. They then used propensity score matching to compare Overall Survival between the adjuvant chemotherapy and postoperative observation groups. Patients included in the study were diagnosed to have clinical stage T1,N1-3,M0 or T2-4,N0-3,M0 adenocarcinoma of the distal esophagus or gastric cardia, between 2006 and 2013, and were treated with preoperative chemoradiotherapy and surgical resection with a curative intent. Patients receiving adjuvant chemotherapy were younger and were more likely to have advanced disease and shorter postoperative hospitalization. A total of 732 patients in the adjuvant chemotherapy group were matched by propensity score to 3660 patients in the postoperative observation group.
It was noted that adjuvant chemotherapy was associated with improved Overall Survival compared with postoperative observation without adjuvant chemotherapy (median survival 40 months versus 34 months; HR=0.79, P <0.001). The Overall Survival at 1, 3, and 5 years was 94%, 54%, and 38% in the adjuvant chemotherapy group and 88%, 47%, and 34% in the observation group, respectively. The survival benefit with adjuvant chemotherapy was noted in most patient subgroups.
Based on this analysis it was concluded that for patients with locally advanced GastroEsophageal adenocarcinoma treated with preoperative chemoradiotherapy and surgical resection, adjuvant chemotherapy was associated with improved Overall Survival. Adjuvant Chemotherapy vs Postoperative Observation Following Preoperative Chemoradiotherapy and Resection in Gastroesophageal Cancer. A Propensity Score–Matched Analysis. Mokdad AA, Yopp AC, Polanco PM, et al. JAMA Oncol. 2018;4:31-38
OGIVRI® (Trastuzumab-dkst)
The FDA on December 1, 2017 approved OGIVRI® as a Biosimilar to HERCEPTIN® (Trastuzumab, Genentech, Inc.) for the treatment of patients with HER2-overexpressing breast or metastatic stomach cancer (Gastric or GastroEsophageal junction adenocarcinoma). OGIVRI® is a product of Mylan N.V.
FDA Approves OGIVRI® as a Biosimilar to HERCEPTIN®
SUMMARY: The FDA on December 1, 2017 approved OGIVRI® (Trastuzumab-dkst) as a biosimilar to HERCEPTIN® (Trastuzumab), for the treatment of patients with HER2-overexpressing breast or metastatic stomach cancer (gastric or gastroesophageal junction adenocarcinoma). It is estimated that 252,710 new cases of invasive breast cancer and 63,410 new cases of non-invasive breast cancer will be diagnosed in women in 2017 and 28,000 new cases of stomach cancer will be diagnosed during this same period. Approximately 20-25% of primary breast cancers are HER2-positive. The frequency of HER2 overexpression in gastric and gastroesophageal cancer is about 18% with the frequency ranging from 4% to 53%.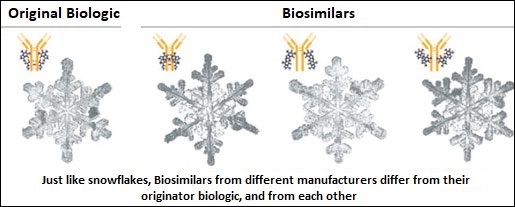
Biosimilar product is a biological product that is approved based on its high similarity to an already approved biological product (also known as reference product). Biological products are made from living organisms including humans, animals and microorganisms such as bacteria or yeast and are manufactured through biotechnology, derived from natural sources or produced synthetically. Biological products have larger molecules with a complex structure than conventional drugs (also known as small molecule drugs). Unlike biological products, conventional drugs are made of pure chemical substances and their structures can be identified. A generic drug is a copy of brand name drug and has the same active ingredient and is the same as brand name drug in dosage form, safety and strength, route of administration, quality, performance characteristics and intended use. Therefore, brand name and the generic drugs are bioequivalent. The Affordable Care Act in 2010 created an abbreviated licensure pathway for biological products that are demonstrated to be “Biosimilar” to, or “interchangeable” with an FDA-licensed (FDA approved) biological product (reference product). The Biosimilar must show that it has no clinically meaningful differences in terms of safety and effectiveness from the reference product. A Biosimilar product can only be approved by the FDA if it has the same mechanism of action, route of administration, dosage form and strength as the reference product, and only for the indications and conditions of use that have been approved for the reference product. Biosimilars are not as easy to manufacture as generics (copies of brand name drugs) because of the complexity of the structure of the biologic product and the process used to make a biologic product. The facilities where Biosimilars are manufactured must also meet the FDA’s standards.
The approval of OGIVRI® was based on comparisons of extensive structural and functional product characterization, animal data, human pharmacokinetic and pharmacodynamic data, and clinical studies including clinical immunogenicity between OGIVRI® and HERCEPTIN®. Heritage is a double-blind, randomized phase III trial in which the efficacy and safety of OGIVRI® , a Biosimilar, was compared with HERCEPTIN®. The randomization included 500 patients treated at 95 sites worldwide, with centrally confirmed, measurable HER2 positive metastatic breast cancer, who had not received prior chemotherapy or HERCEPTIN® for their metastatic disease. Patients received either OGIVRI® or HERCEPTIN® along with TAXOTERE® (Docetaxel) or TAXOL® (Paclitaxel) administered every 3 weeks for a minimum of 8 cycles (24 weeks), with the antibody therapy continued, until disease progression. Both antibodies were administered with a loading dose of 8 mg/kg and a maintenance dose of 6 mg/kg every 3 weeks. Approximately 44% of the enrolled patients had hormone receptor positive disease and 84% received TAXOTERE®. The final analysis included 458 patients of whom 230 were in the OGIVRI® group and 228 were in the HERCEPTIN® group. The Primary endpoint was Overall Response Rate (ORR) at 24 weeks and Secondary endpoints include Progression Free Survival (PFS), Overall Survival (OS) and Safety.
The ORR after 24 weeks of treatment was 69.6% for the OGIVRI® group and 64% for the HERCEPTIN® group and this was not statistically significant. The median PFS had not yet been reached. Safety data in both treatment groups were comparable and there was no significant change in cardiac function from baseline to Week 24 in either group. Safety data were also comparable. The dose-normalized maximum concentration, and Area Under the Curve (AUC), were similar for both antibodies.
The authors concluded that OGIVRI® is equivalent to HERCEPTIN®, when given in combination with a Taxane, as first line therapy, for patients with HER2 positive metastatic breast cancer. Heritage: A phase III safety and efficacy trial of the proposed trastuzumab biosimilar Myl-1401O versus Herceptin. Rugo HS, Barve A, Waller CF, et al. J Clin Oncol 34, 2016 (suppl; abstr LBA503)
MisMatch Repair Deficiency and MicroSatellite Instability May Predict Perioperative Chemotherapy Benefit in Operable GastroEsophageal Cancers
SUMMARY: The American Cancer Society estimates that about 28,000 new cases of stomach cancer will be diagnosed in the United States for 2017 and about 10,960 people will die of this disease. It is a leading cause of cancer-related deaths in the world. Patients with operable Gastric or GastroEsophageal adenocarcinoma frequently receive perioperative or neoadjuvant chemotherapy prior to surgical resection, as this has been associated with a modest improvement in Overall Survival (OS), compared with surgery alone. However, approximately 50% of the patients undergoing surgical resection will die of recurrent disease. Further perioperative chemotherapy can be associated with significant toxicities. For patients with GastroEsophageal cancer receiving neoadjuvant treatment, there are presently no validated prognostic biomarkers, and patient selection is based on preoperative clinical staging.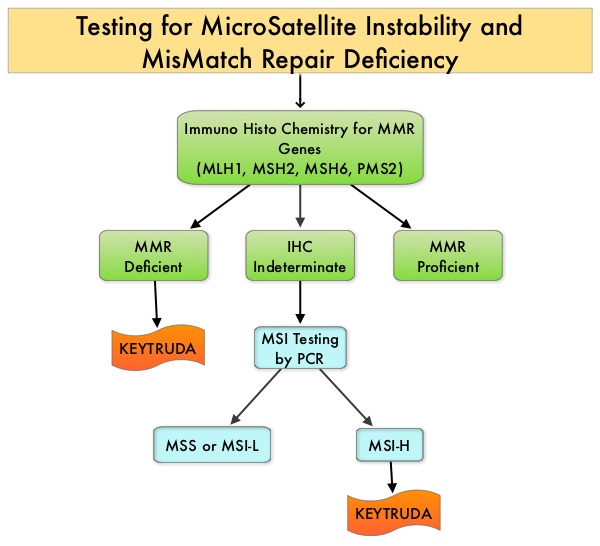
The DNA MisMatchRepair (MMR) system is responsible for molecular surveillance and works as an editing tool that identifies errors within the microsatellite regions of DNA and removes them. Defective MMR system leads to MSI (Micro Satellite Instability) and hypermutation, triggering an enhanced antitumor immune response. MSI (Micro Satellite Instability) is therefore a hallmark of defective/deficient DNA MisMatchRepair (MMR) system and occurs in 15% of all colorectal cancers. Defective MisMatchRepair can be a sporadic or heritable event. Approximately 65% of the MSI colon tumors are sporadic and when sporadic, the DNA MisMatchRepair gene is MLH1. Defective MisMatchRepair can also manifest as a germline mutation occurring in 1 of the 4 MisMatchRepair genes which include MLH1, MSH2, MSH6, PMS2. This produces Lynch Syndrome (Hereditary Nonpolyposis ColoRectal Carcinoma – HNPCC), an autosomal dominant disorder and is the most common form of hereditary colon cancer, accounting for 35% of the MSI colorectal cancers. MSI tumors tend to have better outcomes and this has been attributed to the abundance of Tumor Infiltrating Lymphocytes in these tumors, from increased immunogenicity. These tumors are susceptible to PD-1 blockade and respond to treatment with checkpoint inhibitors such as KEYTRUDA® (N Engl J Med 372:2509-2520, 2015). Other MSI-High and dMMR (MMR deficient) tumors include, Endometrial and GastroIntestinal tumors and to a lesser extent Breast, Prostate, Bladder and Thyroid tumors.
MSI (Micro Satellite Instability) testing is performed using a PCR based assay and MSI-High refers to instability at 2 or more of the 5 mononucleotide repeat markers and MSI-Low refers to instability at 1 of the 5 markers. Patients are considered Micro Satellite Stable (MSS) if no instability occurs. MSI-L and MSS are grouped together because MSI-L tumors are uncommon and behave similar to MSS tumors. Tumors considered MSI-H have deficiency of one or more of the DNA MisMatchRepair genes. MMR gene deficiency can be detected by ImmunoHistoChemistry (IHC). MLH1 gene is often lost in association with PMS2. Approximately 10-20% of Gastric cancers are MSI high or MMR Deficient. Several retrospective studies have suggested favorable outcomes in patients with Gastric cancer with high MSI tumors, although none of these studies had a control group.
In the MAGIC trial (The UK Medical Research Council Adjuvant Gastric Infusional Chemotherapy), which is an open-label, multicenter, phase III study, patients with resectable GastroEsophageal cancer were randomized to receive either 6 cycles of perioperative Epirubicin, Cisplatin, and Infusional 5-FU (3 cycles before and 3 cycles after resection) plus surgery, or undergo surgery alone. In this study, patients treated with perioperative chemotherapy had improved Overall Survival (OS) compared with patients treated with surgery alone (5-year OS 36% versus 23%; HR=0.75; P=0.009).
The authors in this study additionally evaluated patients with operable GastroEsophageal cancers with High MicroSatellite Instability (MSI-H) or MMR deficiency (dMMR), and compared their survival with patients who had MicroSatellite Stable (MSS) GastroEsophageal cancer, when these patients were treated with surgery alone or surgery plus perioperative chemotherapy. The authors thus assessed survival outcomes based on MSI/MMR deficiency. Of the 503 clinical trial participants, MSI results were available for 303 patients and both MSI and MMR results were available in 254 patients. Patients who had High MSI or MMR deficiency treated with surgery alone, had a median OS that was Not Reached (NR) compared with a median Overall Survival (OS) of 20.5 months, among those who had neither high MSI nor MMR deficiency (HR=0.42; P=0.09). In contrast, patients who had either a High MSI or MMR deficiency, treated with surgery plus perioperative chemotherapy had a median OS of 9.6 months compared with a median OS of 19.5 months, among those who had neither High MSI nor MMR deficiency (HR=2.18; P=0.03). The overall concordance rate between MSI-H and MMR deficient status was 97.6%.
Based on these findings the authors concluded that patients with operable GastroEsophageal cancer with High MicroSatellite Instability or MMR deficiency, did not benefit from perioperative chemotherapy and could be spared from the toxicities of chemotherapy. These patients may benefit from therapy with PD-1 inhibitors, although this will need to be further investigated. If independently validated, MSI or MMR deficiency, determined by preoperative biopsies, could be used to select patients for perioperative chemotherapy. Mismatch Repair Deficiency, Microsatellite Instability, and Survival. An Exploratory Analysis of the Medical Research Council Adjuvant Gastric Infusional Chemotherapy (MAGIC) Trial. Smyth EC, Wotherspoon A, Peckitt C, et al. JAMA Oncol. 2017;3:1197-1203.
KEYTRUDA® (Pembrolizumab)
The FDA on September 22, 2017 granted accelerated approval to KEYTRUDA® for patients with recurrent locally advanced or metastatic, Gastric or GastroEsophageal Junction adenocarcinoma, whose tumors express PD-L1, as determined by an FDA-approved test. KEYTRUDA® is a product of Merck & Co., Inc.
FDA Approves KEYTRUDA® for Advanced Gastric Cancer
SUMMARY: The FDA on September 22, 2017 granted accelerated approval to KEYTRUDA® (Pembrolizumab), for patients with recurrent locally advanced or metastatic, Gastric or GastroEsophageal junction adenocarcinoma, whose tumors express PD-L1, as determined by an FDA-approved test. Patients must have had disease progression on or after two or more prior systemic therapies, including Fluoropyrimidine and platinum-containing chemotherapy and, if appropriate, HER2/neu-targeted therapy. Cancers of the esophagus and stomach are among the most prevalent malignancies and are a major cause of cancer-related mortality. It is estimated that in 2016 GastroEsophageal Adenocarcinoma (GEA) accounted for 43,280 new cases in the United States. The incidence of these tumors has been on the rise in the past decade. Majority of the patients with GEA have advanced disease at the time of initial presentation and have limited therapeutic options with little or no chance for cure. Patients with localized disease (stage II and stage III) are often treated with multimodality therapy and 40% of the patients may survive for 5 years or more.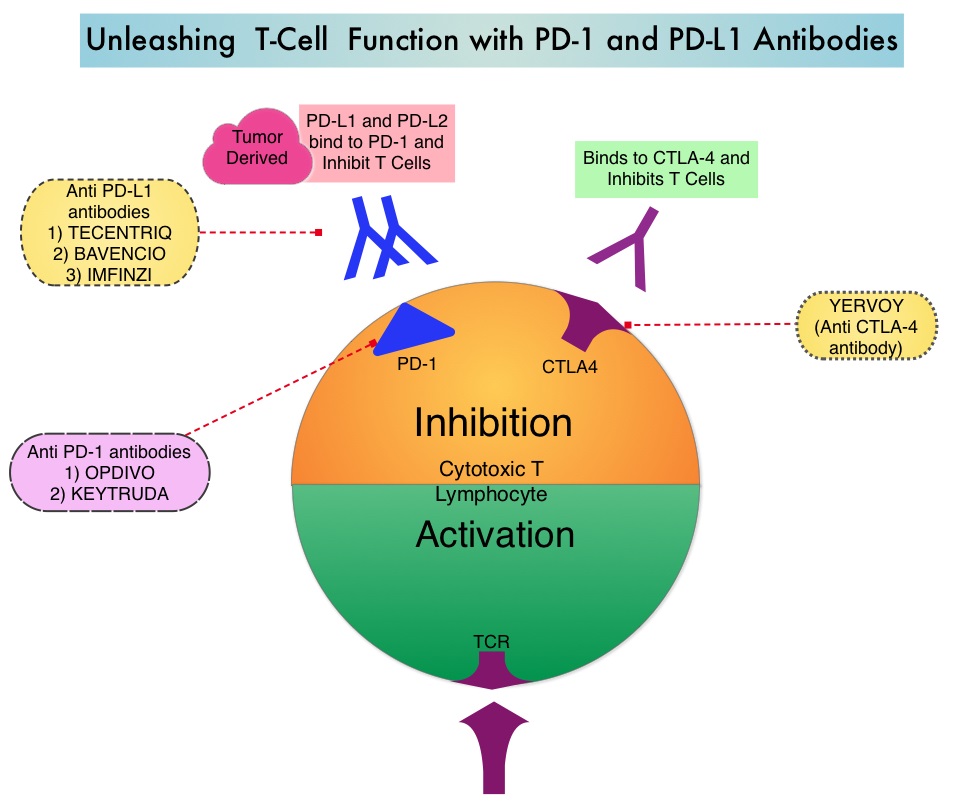
KEYTRUDA® is a fully humanized, Immunoglobulin G4, anti-PD-1, monoclonal antibody, that binds to the PD-1 receptor and blocks its interaction with ligands PD-L1 and PD-L2, thereby undoing PD-1 pathway-mediated inhibition of the immune response and unleashing the tumor-specific effector T cells. In previously reported Phase I study, KEYTRUDA® showed promising antitumor activity with manageable safety, in patients with previously treated advanced gastric cancer.
Based on these findings, the authors conducted a global, multicohort, Phase II study (KEYNOTE 059), in which patients with advanced gastric or gastroesophageal junction cancer received KEYTRUDA® 200 mg every 3 weeks for up to 2 years or until disease progression or unacceptable toxicity. Cohort 1 in this study enrolled 259 patients of whom 57% (N=148) had PD-L1 positive tumors and these tumors were either MicroSatellite Stable (MSS), or had undetermined MicroSatellite Instability (MSI) or MisMatch Repair (MMR) status. PD-L1 expression was evaluated by the PD-L1 IHC (22C3 antibody) and PD-L1 positivity was based on a Combined Positive Score (CPS) of 1 or more. CPS is determined by the number of PD-L1 staining cells (tumor cells, lymphocytes, macrophages) divided by total number of tumor cells evaluated, multiplied by 100. The median age was 62 years, 76% were men and over 50% of the patients received KEYTRUDA® as third line treatment or beyond. The median duration of follow up was 5.4 months. Primary end points included Objective Response Rate (ORR), safety, and tolerability.
In the group of patients with PD-L1 positive tumors, the ORR was 15.5% with 2% Complete Responses and 13.5% Partial Responses. Among the responding patients, the response duration ranged from 3-19 months, with 58% of the responding patients having response durations of 6 months or longer and 26% of the responding patients having response durations of 12 months or longer. In this cohort of 259 patients, 3% had tumors that were determined to be MSI-High. The ORR in this group was 57%, with response duration ranging from 5-14 months. In the PD-L1 negative patients however, the ORR was only 5.5%.
It was concluded that KEYTRUDA® demonstrated promising antitumor activity and durable responses in patients with advanced Gastric/GastroEsophageal Junction cancer, who had progressed on more than 2 lines of therapy, with higher Objective Response Rates noted in patients with PD-L1-positive tumors. KEYNOTE-059 cohort 1: Efficacy and safety of pembrolizumab (pembro) monotherapy in patients with previously treated advanced gastric cancer. Fuchs CS, Doi T, Jang RW-J, et al. J Clin Oncol. 2017;35 (suppl; abstr 4003).
Guideline for HER2 Testing in Gastroesophageal Adenocarcinoma
SUMMARY: It is estimated that in 2016 GastroEsophageal Adenocarcinoma (GEA) accounted for 43,280 new cases in the United States. Majority of the patients with GEA have advanced disease at the time of initial presentation and have limited therapeutic options with little or no chance for cure. Patients with localized disease (stage II and stage III) are often treated with multimodality therapy and 40% of the patients may survive for 5 years or more. Approximately 7-38% of GEAs have amplification and/or overexpression of HER2. HER2 (ERBB2) is a proto-oncogene located on the long arm of chromosome 17 (17q12) that encodes a tyrosine kinase receptor, which upon dimerization and phosphorylation, initiates signaling pathways, that lead to cell division, proliferation, differentiation and anti-apoptosis signaling.
GastroEsophageal junction tumors have a higher incidence of overexpression of HER2 compared to gastric cancers. In the stomach, overexpression of HER2 varies with histologic type (intestinal-type having greater expression than diffuse-type) and differentiation (well and moderately differentiated tumors having greater expression than poorly differentiated tumors). Further, the heterogeneity of immunostaining is greater in GEA and the complete membrane staining required for positivity in breast cancer, is not common in GEA. Due to the high heterogeneity of a gastric cancer, it is appropriate to evaluate HER2 expression on biopsy specimens, especially in unresectable cases and reevaluate it on resected specimens, when available.
The NCCN (National Comprehensive Cancer Network) Clinical Practice Guidelines in Oncology for Gastric Cancer and Esophageal and Esophagogastric Junction Cancers, recommend assessment of HER2 overexpression using ImmunoHistoChemistry and/or gene amplification using FISH (Fluorescence In Situ Hybridization or another in situ hybridization method, in tumor samples from patients, with unresectable, locally advanced, recurrent, or metastatic GEA, for whom HERCEPTIN® may be potentially beneficial. Testing for HER2 is primarily performed on Formalin-Fixed and Paraffin-Embedded biopsy or resection tumor tissue from the primary or metastatic site. There are important differences in HER2 expression, scoring, and outcomes in GEA compared to breast carcinoma, and the need for HER2 guidelines (that include critical clinical and laboratory considerations) was therefore recognized. The CAP, American Society for Clinical Pathology, and ASCO convened an international expert panel to systematically review published documents and to develop an evidence-based guideline, to establish recommendations for HER2 testing in GastroEsophageal Adenocarcinoma.
HERCEPTIN® (Trastuzumab) is humanized monoclonal antibody that targets HER2. HERCEPTIN® is effective only in cancers where HER2 is overexpressed. In a previously published randomized phase III trial, HERCEPTIN® in combination with chemotherapy was shown to significantly improve Overall Survival compared with chemotherapy alone, in patients with HER2 positive advanced GEA.
The following are the Guideline Summary from the College of American Pathologists, American Society for Clinical Pathology, and American Society of Clinical Oncology
Guideline Questions
• What is the optimal testing algorithm for the assessment of Human Epithelial Growth Factor 2 (HER2) status in patients with GastroEsophageal Adenocarcinoma (GEA)?
• What strategies can help ensure optimal performance, interpretation, and reporting of established assays in patients with GEA?
Target Population: Patients with GEA.
Target Audience: Medical and surgical oncologists; oncology nurses and physician assistants; pathologists; general practitioners; and patients.
Key Points and Recommendations for Clinicians
Recommendation 1.1
For patients with advanced GEA who are potential candidates for HER2-targeted therapy, the treating clinician should request HER2 testing on tumor tissue.
Recommendation 1.2
Treating clinicians or pathologists should request HER2 testing on tumor tissue in the biopsy or resection specimens (primary or metastasis) preferably before the initiation of HERCEPTIN® therapy if such specimens are available and adequate. HER2 testing on fine-needle aspiration specimens (cell blocks) is an acceptable alternative.
Recommendation 1.3
Treating clinicians should offer combination chemotherapy and HER2-targeted therapy as the initial treatment of appropriate patients with HER2-positive tumors who have advanced GEA
Key Points and Recommendations for Pathologists
Recommendation 2.1
Laboratories/pathologists must specify the antibodies and probes used for the test and ensure that assays are appropriately validated for HER2 ImmunoHistoChemistry (IHC) and in situ hybridization (ISH) on GEA specimens.
Recommendation 2.2
When GEA HER2 status is being evaluated, laboratories/pathologists should perform/order IHC testing first, followed by ISH (In Situ Hybridization) when the IHC result is 2+ (equivocal). Positive (3+) or negative (0 or 1+) HER2 IHC results do not require further ISH testing.
Recommendation 2.3
Pathologists should use the Ruschoff/Hofmann method in scoring HER2 IHC and ISH results for GEA.
Recommendation 2.4
Pathologists should select the tissue block with the areas of lowest grade tumor morphology in biopsy and resection specimens. More than one tissue block may be selected if different morphologic patterns are present.
Recommendation 2.5
Laboratories should report HER2 test results in GEA specimens in accordance with the College of American Pathologists biomarker Template for Reporting Results of HER2 (ERBB2) Biomarker Testing of Specimens From Patients With Adenocarcinoma of the Stomach or Esophagogastric Junction.
Recommendation 2.6
Pathologists should identify areas of invasive adenocarcinoma and also mark areas with strongest intensity of HER2 expression by IHC in GEA specimens for subsequent ISH scoring when required.
Recommendation 2.7
Laboratories must incorporate GEA HER2 testing methods into their overall laboratory quality improvement program, establishing appropriate quality improvement monitors as needed to ensure consistent performance in all steps of the testing and reporting process. In particular, laboratories performing GEA HER2 testing should participate in a formal proficiency testing program, if available, or an alternative proficiency assurance activity.
Recommendation 2.8
There is insufficient evidence to recommend for or against genomic testing in patients with GEA at this time.
HER2 Testing and Clinical Decision Making in Gastroesophageal Adenocarcinoma: Guideline Summary From the College of American Pathologists, American Society for Clinical Pathology, and American Society of Clinical Oncology. Bartley AN, Washington MK, Ismaila N, et al. Journal of Oncology Practice 2017;13:53-57.
CYRAMZA® (Ramucirumab)
The FDA on November 5, 2014 approved CYRAMZA® for use in combination with TAXOL® (Paclitaxel), for the treatment of patients with advanced Gastric or GastroEsophageal Junction (GEJ) adenocarcinoma. CYRAMZA® was approved in April, 2014 as a single agent for the treatment of patients with advanced Gastric or GEJ adenocarcinoma refractory to or progressive following first-line therapy with platinum or fluoropyrimidine chemotherapy. CYRAMZA® injection for intravenous infusion is a product of Eli Lilly and Company.
RAINBOW A global, phase III, randomized, double-blind study of ramucirumab plus paclitaxel versus placebo plus paclitaxel in the treatment of metastatic gastroesophageal junction (GEJ) and gastric adenocarcinoma following disease progression on first-line platinum- and fluoropyrimidine-containing combination therapy rainbow IMCL CP12-0922 (I4T-IE-JVBE)
SUMMARY: The FDA on November 5, 2014 approved CYRAMZA® (Ramucirumab) for use in combination with TAXOL® (Paclitaxel) for the treatment of patients with advanced gastric or GastroEsophageal Junction (GEJ) adenocarcinoma. CYRAMZA® was approved by the FDA in April, 2014 as a single agent for the treatment of patients with advanced gastric or GEJ adenocarcinoma, refractory to or progressive, following first-line therapy with platinum or fluoropyrimidine chemotherapy. It is estimated that there were approximately 21,600 new cases and 10,990 deaths from gastric cancer in the United States in 2013. The biology of gastric cancer appears to be different in different parts of the globe. Following progression after first line treatment for metastatic disease, the median survival is approximately 3 months. CYRAMZA® is a human IgG1 monoclonal antibody that inhibits VEGF-receptor 2, unlike AVASTIN® (Bevacizumab) which inhibits VEGF-A.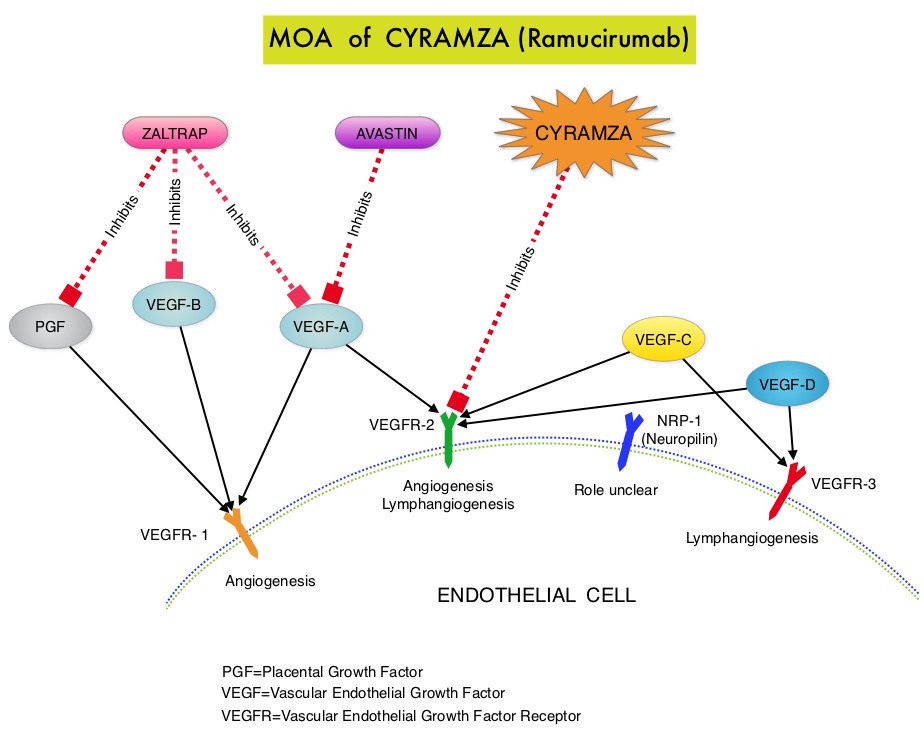 The RAINBOW study is an international, placebo-controlled, double-blind, phase III trial in which 665 patients with metastatic gastroesophageal junction or gastric adenocarcinoma, who had disease progression on or within 4 months after first-line platinum and fluoropyrimidine-based combination therapy, were included. Patients were randomly assigned to receive TAXOL® (Paclitaxel) 80 mg/m2 given on D1, 8, 15 along with Placebo (N=335) or the same dose and schedule of TAXOL® given along with CYRAMZA® at 8 mg/kg IV every 2 weeks (N=330), of a 28 day cycle. Treatment was continued until disease progression or unacceptable toxicities were noted. The primary endpoint was Overall Survival (OS). Secondary endpoints included Progression Free Survival (PFS), Objective Response Rate (ORR) and Time To Progression (TTP). The median OS for the combination of CYRAMZA® and TAXOL® was 9.6 months compared to 7.4 months for Placebo and TAXOL® (HR=0.81; P=0.017), resulting in a 19% reduction in the risk of death with the CYRAMZA® and TAXOL® combination. The secondary endpoints favored the CYRAMZA® and TAXOL® combination as well. The median PFS was 4.4 months and 2.9 months (HR=0.64; P<0.001), ORR was 28% and 16% (P<0.0001) and median TTP was 5.5 months and 3 months with the CYRAMZA® and TAXOL® combination vs Placebo and TAXOL® combination respectively. As one would expect, treatment related adverse events were seen more frequently in the CYRAMZA® and TAXOL® combination group. Significant were neutropenia, hypertension, fatigue and asthenia, diarrhea and epistaxis. The incidence of febrile neutropenia in the two treatment groups was however comparable (3.1% vs 2.4%). The authors concluded that the combination of CYRAMZA® and TAXOL® combination significantly improved both Progression Free and Overall Survival and also resulted in significantly improved disease control rates, in patients with metastatic gastroesophageal junction or gastric adenocarcinoma. Wilke H, Van Cutsem E, Oh SC, et al. J Clin Oncol 32, 2014 (suppl 3; abstr LBA7)
The RAINBOW study is an international, placebo-controlled, double-blind, phase III trial in which 665 patients with metastatic gastroesophageal junction or gastric adenocarcinoma, who had disease progression on or within 4 months after first-line platinum and fluoropyrimidine-based combination therapy, were included. Patients were randomly assigned to receive TAXOL® (Paclitaxel) 80 mg/m2 given on D1, 8, 15 along with Placebo (N=335) or the same dose and schedule of TAXOL® given along with CYRAMZA® at 8 mg/kg IV every 2 weeks (N=330), of a 28 day cycle. Treatment was continued until disease progression or unacceptable toxicities were noted. The primary endpoint was Overall Survival (OS). Secondary endpoints included Progression Free Survival (PFS), Objective Response Rate (ORR) and Time To Progression (TTP). The median OS for the combination of CYRAMZA® and TAXOL® was 9.6 months compared to 7.4 months for Placebo and TAXOL® (HR=0.81; P=0.017), resulting in a 19% reduction in the risk of death with the CYRAMZA® and TAXOL® combination. The secondary endpoints favored the CYRAMZA® and TAXOL® combination as well. The median PFS was 4.4 months and 2.9 months (HR=0.64; P<0.001), ORR was 28% and 16% (P<0.0001) and median TTP was 5.5 months and 3 months with the CYRAMZA® and TAXOL® combination vs Placebo and TAXOL® combination respectively. As one would expect, treatment related adverse events were seen more frequently in the CYRAMZA® and TAXOL® combination group. Significant were neutropenia, hypertension, fatigue and asthenia, diarrhea and epistaxis. The incidence of febrile neutropenia in the two treatment groups was however comparable (3.1% vs 2.4%). The authors concluded that the combination of CYRAMZA® and TAXOL® combination significantly improved both Progression Free and Overall Survival and also resulted in significantly improved disease control rates, in patients with metastatic gastroesophageal junction or gastric adenocarcinoma. Wilke H, Van Cutsem E, Oh SC, et al. J Clin Oncol 32, 2014 (suppl 3; abstr LBA7)
