SUMMARY: Colorectal Cancer (CRC) is the third leading cause of cancer-related deaths in men and women in the United States. The American Cancer Society estimates that approximately 149,500 new cases of CRC will be diagnosed in the United States in 2021 and about 52,980 patients will die of the disease. The lifetime risk of developing CRC is about 1 in 23. The majority of CRC cases (about 75 %) are sporadic whereas the remaining 25 % of the patients have family histories of the disease. Only 5-6 % of patients with CRC with a family history background are due to inherited mutations in major CRC genes, while the rest are the result of accumulation of both genetic mutations and epigenetic modifications of several genes. Colorectal Cancer is a heterogeneous disease classified by its genetics, and even though the overall death rate has continued to drop, deaths from CRC among people younger than 55 years have increased 1% per year from 2008 to 2017, with 12% of CRC cases diagnosed in people under age 50.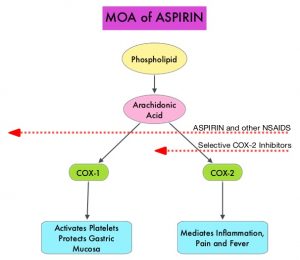
Aspirin (AcetylSalicylic Acid) has been studied as a chemopreventive agent for several decades and the temporal relationship between systemic inflammation and cancer has been a topic of ongoing investigation. The US Preventive Services Task Force (USPSTF) found adequate evidence that Aspirin use reduces the incidence of CRC in adults after 5-10 years of use, and recommends initiating low-dose Aspirin use for the primary prevention of CardioVascular Disease (CVD) and CRC, in adults aged 50-69 years, who have a 10% or greater 10-year CVD risk, are not at increased risk for bleeding, have a life expectancy of at least 10 years, and are willing to take low-dose Aspirin daily for at least 10 years.
The molecular mechanisms underlying Aspirin’s chemoprevention effects as well as the dose, duration, and timing of Aspirin chemoprevention have remained unclear. More recent data suggests that platelets may play a role in tumorigenesis as well, through the release of angiogenic and growth factors due to overexpression of COX-2. Daily low dose Aspirin inhibits COX-1 and COX-2. It is postulated that Aspirin also works by COX-independent mechanisms such as, the inhibition of NF-kB and Wnt/ β-catenin signaling, which may play a role in its chemopreventive properties.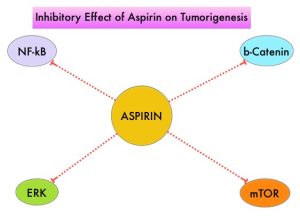
Two recently published studies have provided new information on the association between regular aspirin use, and CRC incidence.
In the first study by Zhang and colleagues, the authors addressed the use of aspirin for the primary prevention of CRC and explored the dosing, timing and duration of Aspirin intake, to reduce the incidence of CRC. The authors derived data from two large US cohort studies, The Nurses’ Health Study (January 1980-June 2014) and the Health Professionals Follow-up Study (January 1986-January 2014). These two studies provided data on the use of Aspirin by more than 94,500 participants over a period of 35 years, providing a unique opportunity to evaluate the chemopreventive benefit of Aspirin on CRC. Colorectal cancer incidence was approximately 10% lower amongst individuals reporting regular Aspirin use immediate 10 years or more earlier before follow up started, with the lowest average dose studied (23-70 mg/day) appearing as effective as higher doses. However, when the period of Aspirin use was between 5 and 10 years earlier, a smaller reduction in CRC incidence was noted amongst those taking aspirin, but the greatest reduction was noted among those taking the highest dose. This study suggested that the benefit necessitates at least 6-10 years and most clearly after approximately 10 years since initiation of Aspirin. Both remote use and use within the previous 10 years contributed independently to decreased risk, though a lower dose may be required for a benefit with longer term use.
Figueiredo and colleagues studied whether the use of Aspirin prior to or after a diagnosis of CRC, affects subsequent cancer-related mortality. They utilized data from men and women enrolled in the American Cancer Society’s Cancer Prevention Study-II (CPS-II) Nutrition Cohort who were cancer-free at the baseline (year 1992/1993), and diagnosed with CRC during follow up through 2015. They compared CRC-specific mortality amongst long-term regular Aspirin users (defined as 15 or more times per month) and non-users prior to and after diagnosis. Long-term regular use of Aspirin before diagnosis was associated with lower CRC mortality. Regular use of Aspirin following diagnosis was not statistically significantly associated with risk of CRC-specific mortality overall, although participants who began regular Aspirin use, only after their diagnosis, were at lower risk, than participants who did not use Aspirin at both the pre-and post-diagnosis periods. Further, long-term Aspirin use before diagnosis was also associated with lower risk of distant metastases. This study suggested that long-term Aspirin use before a diagnosis of non-metastatic CRC may be associated with lower CRC-specific mortality after diagnosis, implying possible inhibition of micro-metastases before diagnosis.
Taken together, the study by Zhang et al. suggested that even a relatively small dose of Aspirin taken regularly for 2-5 years during the middle years of life might reduce the risk of colorectal cancer 10 years or so later, whereas the study by Figueiredo and colleagues suggested that Aspirin, taken prior to (or started after) a diagnosis of colorectal cancer, reduced subsequent metastatic spread and cancer related mortality. Even though these two new studies support the anti-cancer effect of Aspirin, additional consistent information may be required before widespread role of Aspirin for primary prevention of cancer is embraced.
Timing of aspirin use in colorectal cancer chemoprevention: a prospective cohort study. Zhang Y, Chan AT, Meyerhardt JA, et al. J Natl Cancer Inst 2021; https://doi.org/10.1093/jnci/djab009
Associations of aspirin and non-aspirin non-steroidal anti-inflammatory drugs with colorectal cancer mortality after diagnosis. Figueiredo JC, Jacobs EJ, Newton CC, et al. J Natl Cancer Inst 2021; https://doi.org/10.1093/jnci/djab008

