SUMMARY: The FDA on October 18, 2017, granted regular approval to Axicabtagene ciloleucel (YESCARTA®) for the treatment of adult patients with relapsed or refractory Large B-Cell Lymphoma after two or more lines of systemic therapy, including Diffuse Large B-Cell Lymphoma (DLBCL) Not Otherwise Specified, Primary Mediastinal Large B-Cell Lymphoma, High-grade B-Cell Lymphoma, and DLBCL arising from Follicular Lymphoma (Transformed Follicular Lymphoma-TFL).
What is (CAR) T-cell immunotherapy? Chimeric Antigen Receptor (CAR) T-cell therapy is a type of immunotherapy and consists of T cells collected from the patient’s blood in a leukapheresis procedure, and genetically engineered to produce special receptors on their surface called Chimeric Antigen Receptors (CAR). These reprogrammed cytotoxic T cells with the Chimeric Antigen Receptors on their surface are now able to recognize a specific antigen on tumor cells. These genetically engineered and reprogrammed CAR T-cells are grown in the lab and are then infused into the patient. These cells in turn proliferate in the patient’s body and the engineered receptor on the cell surface help recognize and kill cancer cells that expresses that specific antigen. It is a therefore a customized treatment created using patient’s own T cells to destroy cancer cells.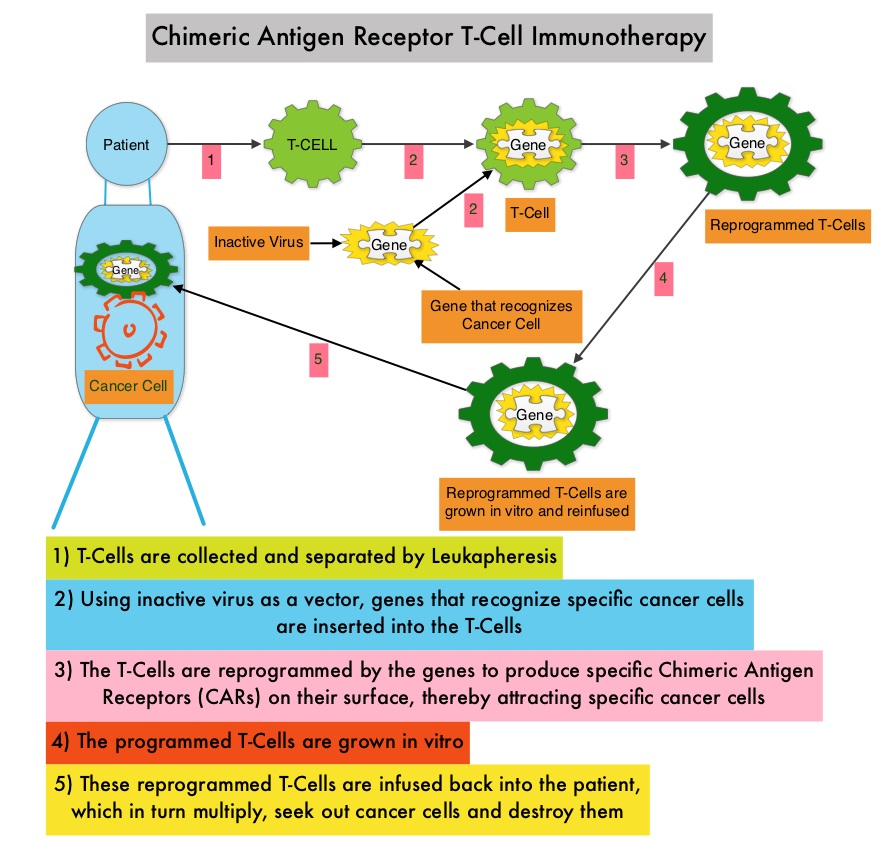
YESCARTA® is a Chimeric Antigen Receptor (CAR) T cell immunotherapy and consists of autologous T cells that are genetically modified to produce a CAR protein, allowing the T cells to seek out and destroy cancer cells expressing the antigen CD19, which is found uniquely on B cells. Patients, following treatment with CAR T-cells, develop B-cell aplasia (absence of CD19 positive cells) due to B-cell destruction and may need immunoglobin replacement. Hence, B-cell aplasia can be a useful therapeutic marker, as continued B-cell aplasia has been seen in all patients who had sustained remission, following CAR T-cell therapy. Cytokine Release Syndrome (CRS), an inflammatory process is the most common and serious side effect of CAR T-cell therapy and is associated with marked elevation of Interleukin-6. Cytokine release is important for T-cell activation and can result in high fevers and myalgias. This is usually self limiting although if severe can be associated with hypotension and respiratory insufficiency. Tocilizumab (ACTEMRA®), an Interleukin-6 receptor blocking antibody produces a rapid improvement in symptoms. This is however not recommended unless the symptoms are severe and life threatening, as blunting the cytokine response can in turn negate T-cell proliferation. Elevated serum Ferritin and C-reactive protein levels are surrogate markers for severe Cytokine Release Syndrome. The CAR T-cells have been shown to also access sanctuary sites such as the central nervous system and eradicate cancer cells. CD19 antigen is expressed by majority of the B cell malignancies and therefore most studies using CAR T-cell therapy have focused on the treatment of advanced B-cell malignancies such as Chronic Lymphocytic Leukemia (CLL), Acute Lymphoblastic Leukemia (ALL) and Non Hodgkin lymphoma (NHL), such as Diffuse Large B-Cell Lymphoma (DLBCL).
Diffuse Large B-Cell Lymphoma (DLBCL) is the most common of the aggressive Non-Hodgkin lymphoma’s in the United States, and the incidence has steadily increased 3 to 4% each year. Outcomes for patients with relapsed/refractory disease is poor, with an Objective response Rate (ORR) of 26%, Complete Response (CR) rate of 8% and a median Overall Survival (OS) of 6.6 months. There is therefore a significant unmet need in this patient group.
The safety and efficacy of YESCARTA® was evaluated in a single arm multicenter clinical trial (ZUMA-1 study) in which 111 patients were enrolled and 101 patients received therapy with YESCARTA®. This study included patients with DLBCL (N=77) and Primary Mediastinal B-Cell Lymphoma (PMBCL)/Transformed Follicular Lymphoma-TFL (N=24), with chemo refractory disease or patients who had relapsed within 12 months post Autologous Stem Cell Transplantation. Following 3 days of conditioning regimen with Cyclophosphamide and Fludarabine, patients received a single infusion of YESCARTA® at a dose of 2 x 106 CAR-positive T cells/kg. The average turnaround time from apheresis to delivery to clinical site for infusion, was 17 days. The Primary end point was Objective Response Rate (ORR) and Secondary endpoints included Duration of Response, Overall Survival and Safety. The preliminary results were reported after the Primary end point was met.
After a median follow up of 8.7 months, the ORR for the entire group was 82% with 54% CR rate (P<0.0001). Among those with DLBCL, the ORR was 82% and the CR rate was 49% and in the PMBCL/TFL group, the ORR was 83% and the CR rate was 71%. At the time of median follow up, 44% of the patients had ongoing responses and the median Duration of Response was 8.2 months and not reached for those in CR. The median Progression Free Survival was 5.9 months and median OS was not reached.
The most common grade 3 or higher adverse reactions included cytopenias, febrile neutropenia, fever, Cytokine Release Syndrome (CRS) and neurologic events. CRS and neurologic events were generally reversible and 43% received Tocilizumb and 27% received steroids and this did not negatively impact outcomes.
The authors concluded that ZUMA-1 is the first pivotal trial of CD19-specific CAR T-cell therapy in patients with refractory aggressive Non Hodgkin Lymphoma, demonstrating significant clinical activity, with a Complete Response rate 7 times higher than the historic control rate. Primary results from ZUMA-1: a pivotal trial of axicabtagene ciloleucel (Axi-cel; KTE-C19) in patients with refractory aggressive non-Hodgkin lymphoma (NHL). Locke FL, Neelapu SS, Bartlett NL, et al. Presented at: 2017 AACR Annual Meeting; April 1-5, 2017; Washington, DC. Abstract CT019.

