SUMMARY: The American Cancer Society estimates that in the United States for 2018, about 8,500 new cases of Hodgkin Lymphoma will be diagnosed and about 1,050 patients will die of the disease. Hodgkin Lymphoma is classified into two main groups – Classical Hodgkin Lymphomas and Nodular Lymphocyte Predominant type, by the World Health Organization. The Classical Hodgkin Lymphomas include Nodular sclerosing, Mixed cellularity, Lymphocyte rich, Lymphocyte depleted subtypes and accounts for approximately 10% of all malignant lymphomas. Nodular sclerosis Hodgkin Lymphoma histology, accounts for approximately 80% of Hodgkin lymphoma cases in older children and adolescents in the United States. Classical Hodgkin Lymphoma is a malignancy of primarily B lymphocytes and is characterized by the presence of large mononucleated Hodgkin (H) and giant multinucleated Reed-Sternberg (RS) cells, collectively known as Hodgkin and Reed-Sternberg cells (HRS).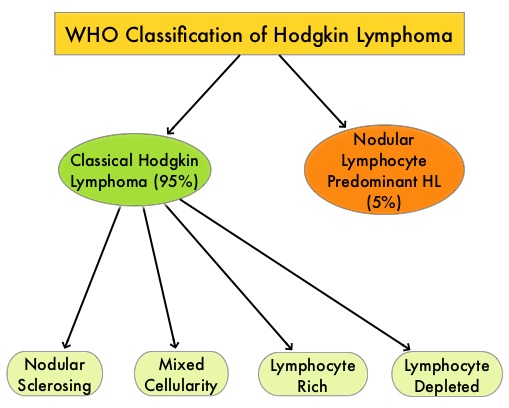
For patients with Hodgkin Lymphoma, the goal of first-line chemotherapy is cure. A positive PET scan following first-line chemotherapy is indicative of incomplete response with residual disease and warrants subsequent chemotherapy or radiation. Advanced stage (Stage III-IV) Classical Hodgkin Lymphoma has a cure rate of approximately 70-80% when treated in the first-line setting with a combination of Doxorubicin, Bleomycin, Vinblastine, and Dacarbazine (ABVD). This regimen which was developed more than 40 years ago is less expensive, easy to administer, is generally well tolerated and is often used in first line setting. Nonetheless, this regimen which contains Bleomycin can cause pulmonary toxicity, the incidence of which is higher in older patients and in those who receive consolidation radiotherapy to the thorax.
ADCETRIS® (Brentuximab vedotin) is an Antibody-Drug Conjugate (ADC) that targets CD30, which is a surface antigen, expressed on Reed-Sternberg cells, in patients with Classical Hodgkin Lymphoma. This ADC consists of an anti-CD30 monoclonal antibody linked to MonoMethyl Auristatin E (MMAE), an antimicrotubule agent. Upon binding to the CD30 molecule on the cancer cells, MMAE is released into the cancer cell, resulting in cell death. ADCETRIS® is presently approved by the FDA for previously untreated Stage III or IV Classical Hodgkin Lymphoma (cHL), in combination with chemotherapy, for treatment of Classical Hodgkin lymphoma at high risk of relapse or progression, as post-autologous Hematopoietic Stem Cell Transplantation (auto-HSCT) consolidation, and for treatment of Classical Hodgkin Lymphoma after failure of auto-HSCT or after failure of at least two prior multi-agent chemotherapy regimens, in patients who are not auto-HSCT candidates.
ECHELON-1 study, which is an international, open-label, randomized, multicenter, phase III trial, compared A+AVD with ABVD, as frontline therapy in patients with Stage III or IV Classical Hodgkin Lymphoma. This study included 1334 previously untreated patients with Stage III or IV Classical Hodgkin Lymphoma, who were randomly assigned in a 1:1 ratio to receive A+AVD (N=664), which consisted of ADCETRIS® 1.2 mg/kg , Doxorubicin 25 mg/m2, Vinblastine 6 mg/m2 and Dacarbazine 375 mg/m2 or ABVD (N=670), which consisted of Doxorubicin 25 mg/m2, Bleomycin 10 units/m2, Vinblastine 6 mg/m2 and Dacarbazine 375 mg/m2, given intravenously on days 1 and 15 of each 28-day cycle, for up to 6 cycles. The Primary end point was “modified” Progression Free Survival (mPFS), defined as progression, death, or the receipt of additional treatment, for patients not achieving CR at the completion of frontline therapy. It was previously reported that at a median follow up of 24.6 months, the 2 year modified PFS in the A+AVD and ABVD groups were 82.1% and 77.2% respectively (HR=0.77; P=0.04), suggesting an approximately 5% benefit with A+AVD.
The North American subgroup analysis of the ECHELON-1 study was conducted because of potential regional differences in the outcomes in the primary study and mPFS benefit was not equally distributed globally. The authors in this prespecified analysis examined the efficacy and safety of A+AVD vs ABVD in North America, as these patients accounted for approximately 40% of the over 1300 patients included in the ECHELON-1 study. This population group included 497 North American patients with advanced Classical Hodgkin Lymphoma, randomized 1:1 to receive up to six cycles of A+AVD or ABVD.
This subgroup analysis revealed an absolute difference of 10.6% in the mPFS per IRF-Independent Review Facility (A+AVD and ABVD groups were 84.3% and 73.7% respectively, HR=0.60; P=0.012) and an 11.7% difference in PFS per investigator review (A+AVD and ABVD groups were 88.1% and 76.4% respectively, HR=0.50; P=0.002), at 2 years. This analysis suggested that a larger proportion of patients in North America benefitted with the A+AVD regimen (10%-12% in North America as opposed to 5% globally). It is postulated that there may be biologic differences in the disease, regional differences in drug metabolism and differences in practice patterns, between countries. Toxicity profile was similar globally. There was a higher incidence of neutropenia in the A+AVD group and G-CSF prophylaxis should be a part of the regimen when A+AVD is used, in contrast to ABVD. Use of G-CSF primary prophylaxis was associated with a lower rate of ADCETRIS® dose delays and dose reductions compared to those without. There was a higher incidence of peripheral neuropathy in the A+AVD group as well, with majority of these events being grade 1 and 2, and this improved or resolved over time. Pulmonary toxicity was lower in patients receiving A+AVD compared to those receiving ABVD.
It was concluded that for patients treated in North America on the ECHELON-1 trial, the absolute difference between A+AVD and ABVD at 2 years for mPFS by IRF was 10.6% and for PFS per Investigator review was 11.7% (10%-12% benefit in North America as opposed to 5% globally). A prospective clinical trial is planned in advanced stage Hodgkin Lymphoma patients treated with A+AVD, to confirm these safety and efficacy findings, in the North American community setting. Brentuximab vedotin (BV) plus chemotherapy in patients with newly diagnosed advanced stage Hodgkin lymphoma (HL): North American results. Ramchandren R, Advani RH, Ansell SM, et al. J Clin Oncol.2018;36(suppl; abstr 7541). doi: 10.1200/JCO.2018.36.15.
