The FDA on April 13, 2021, granted accelerated approval to TRODELVY® for patients with locally advanced or metastatic Urothelial Cancer (mUC) who previously received a Platinum-containing chemotherapy and either a Programmed Death receptor-1 (PD-1) or a Programmed Death-Ligand 1 (PD-L1) inhibitor. TRODELVY® is a product of Immunomedics Inc.
Tag: Urothelial Cancer (Bladder-Ureters-Renal-Pelvis)
PADCEV® Prolongs Overall Survival in Metastatic Urothelial Carcinoma
SUMMARY: The American Cancer Society estimates that in 2021, approximately 83,730 new cases of Bladder Cancer will be diagnosed and 17,200 patients will die of the disease. Patients with urothelial carcinoma are currently treated in the first line setting with a Platinum based chemotherapy regimen and a checkpoint Inhibitor (PD-1 or PD-L1 inhibitor) in the second line setting. Treatment options for patients who progress after first and second line therapies are limited, with poor outcomes. The response rates with standard chemotherapy in this patient population, is about 10%.
PADCEV® (Enfortumab vedotin-ejfv) is an Antibody-Drug Conjugate (ADC) that targets Nectin-4, a cell adhesion molecule highly expressed in urothelial cancers and other solid tumors. Nectin-4 has been implicated in tumor cell growth and proliferation. Following binding to Nectin-4 on the cell surface, PADCEV® becomes internalized and is processed by lysosomes, with the liberation of its cytotoxic payload, Monomethyl auristatin E, which in turn disrupts microtubule assembly, leading to cell cycle arrest and apoptosis. The FDA in 2019 granted accelerated approval to PADCEV® for adult patients with locally advanced or metastatic urothelial cancer, who have previously received a Programmed Death receptor-1 (PD-1) or Programmed Death-Ligand1 (PD-L1) inhibitor, and a Platinum-containing chemotherapy in the neoadjuvant/adjuvant, locally advanced or metastatic setting. This approval was based on the results from the pivotal Phase II EV-201 study which concluded that treatment with PADCEV® demonstrated a clinically meaningful 44% Objective Response Rate (ORR) in this patient group. EV-301 study was designed to confirm the clinical benefit of PADCEV® as compared with standard chemotherapy, by assessing Overall Survival in patients with advanced urothelial carcinoma, who had previously received treatment.
EV-301 is a global, open-label, randomized, Phase III trial, that evaluated the efficacy of PADCEV®, as compared with chemotherapy, in patients with locally advanced or metastatic urothelial carcinoma, who had previously received treatment with a platinum-based chemotherapy and a PD-1 or PD-L1 inhibitor. A total of 608 patients were randomly assigned 1:1 to receive either PADCEV® 1.25 mg/kg IV on days 1, 8, and 15 of a 28-day cycle (N=301), or investigator choice of chemotherapy (Docetaxel 75 mg/m2 IV, Paclitaxel 175 mg/m2 IV, or Vinflunine 320 mg/m2 IV, administered on day 1 of a 21-day cycle (N=307). Both treatment groups were well balanced. The median patient age was 68 years, about 79% of patients had visceral metastases, and 69% of patients had no response to previous treatment with checkpoint inhibitor. The Primary end point was Overall Survival (OS). Secondary end points included Progression Free Survival (PFS) and Overall Response Rate (ORR) and Safety. At the prespecified interim analysis, the median follow up was 11.1 months.
The median OS was 12.88 months in the PADCEV® group versus 8.97 months in patients treated with chemotherapy (H= 0.70; P=0.001), suggesting a 30% reduction in the risk of death with PADCEV®. The PFS was also longer in the PADCEV® group, and was 5.6 months versus 3.7 months with chemotherapy (HR=0.62; P<0.001). The confirmed ORR was higher in the PADCEV® group than in the chemotherapy group (40.6% versus 17.9%; P<0.001), and a Complete Response was observed in 4.9% of the patients in the PADCEV® group and in 2.7% of the patients in the chemotherapy group. Disease Control Rate was 71.9% and 53.4%, respectively (P<0.001). Treatment-related Adverse Events were similar in the two treatment groups.
The authors concluded that treatment with PADCEV® resulted in significantly longer Overall Survival, Progression Free Survival and a higher Overall Response Rate, than standard chemotherapy, in patients with locally advanced or metastatic urothelial carcinoma, who had previously received Platinum-based treatment and a PD-1 or PD-L1 inhibitor.
Enfortumab Vedotin in Previously Treated Advanced Urothelial Carcinoma. Powles T, Rosenberg JE, Sonpavde GP, et al. N Engl J Med 2021; DOI: 10.1056/NEJMoa2035807
Late Breaking Abstract – ASCO 2020: FDA Approves BAVENCIO® for Maintenance Treatment in Advanced Urothelial Carcinoma
SUMMARY: The FDA on June 30, 2020 approved BAVENCIO® for maintenance treatment of patients with locally advanced or metastatic Urothelial Carcinoma (UC) that has not progressed with first-line platinum-containing chemotherapy. The American Cancer Society estimates that for 2020, about 81,400 new cases of bladder cancer will be diagnosed in the US and about 17,980 patients will die of the disease. Bladder cancer is the fourth most common cancer in men, but is less common in women, and the average age at the time of diagnosis is 73. Patients with advanced Urothelial Carcinoma are currently treated in the first line setting with a Platinum based chemotherapy regimen. Progression Free Survival (PFS) and Overall Survival (OS) however are generally short because of resistance to chemotherapy. Treatment options for patients who progress after Platinum based chemotherapy are limited, with poor outcomes. The response rates with standard chemotherapy in this patient population, is about 10%.
BAVENCIO® (Avelumab) is a human, immunoglobulin G1 lambda, PD-L1 targeted monoclonal antibody that binds to PD-L1 and blocks the interaction between PD-L1 and its receptor PD-1. This in turn negates the inhibitory effects of PD-L1 on the immune response by unleashing the immune system and restoring antitumor immune responses. In addition, BAVENCIO® induces Antibody Dependent Cell-mediated Cytotoxicity (ADCC). BAVENCIO® was previously granted an accelerated approval by the FDA in 2017 for the treatment of patients with locally advanced or metastatic Urothelial Carcinoma who have disease progression during or following Platinum-containing chemotherapy.
JAVELIN Bladder 100 study is an international, multicenter, open-label, parallel-arm, randomized Phase III trial, which evaluated BAVENCIO® as maintenance therapy following response or stable disease with first-line Platinum-based chemotherapy, in patients with advanced Urothelial Carcinoma. This study included 700 patients with unresectable locally advanced or metastatic Urothelial Cancer, whose disease did not progress following 4 to 6 cycles of standard Gemcitabine with either Cisplatin or Carboplatin. These patients were randomly assigned 1:1 to receive maintenance BAVENCIO® 10 mg/kg IV every 2 weeks in 4 week cycles plus Best Supportive Care (N=350) or BSC alone (N=350). Best Supportive Care included symptom control and pain management, supportive nutrition, correction of metabolic disorders and antibiotics if indicated. Patients were stratified by best response to first-line chemotherapy (Complete vs Partial Response vs stable disease), and by visceral vs non-visceral disease, when initiating first-line chemotherapy. Across the study population, 51% of patients had tumors that were PD-L1 positive. The Coprimary end points were Overall Survival (OS) in all randomized patients, and in those with PD-L1 positive tumors. Secondary end points included Progression Free Survival (PFS), Objective Response Rate (ORR), and safety. The median follow up was 19.6 months for the BAVENCIO® cohort and 19.2 months for the BSC-alone cohort.
The combination of BAVENCIO® plus BSC significantly prolonged OS, compared with BSC alone, in all randomized patients (HR=0.69; P=0.0005), suggesting a 31% reduction in the risk of death with the addition of maintenance BAVENCIO®. The median OS was 21.4 months with BAVENCIO® plus BSC compared with 14.3 months with BSC alone. Significantly prolonged OS with BAVENCIO® plus BSC, compared with BSC alone, was also noted among patients with PD-L1 positive tumors, and the median OS was not reached in the BAVENCIO® group versus 17.1 months in the control group (HR=0.56; P=0.0003). The OS benefit with BAVENCIO® was noted across all prespecified subgroups, including those defined by Cisplatin-based or Carboplatin-based chemotherapy, and regardless of whether response or stable disease was reached after first-line induction chemotherapy. Based on blinded Independent Central Review, the median PFS favored the BAVENCIO® group both in the overall randomized population (3.7 months versus 2 months, HR=0.62; P<0.001) as well as in the PD-L1 positive subgroup (HR=0.56). All-grade Adverse Events occurred in 98% of the BAVENCIO® group versus 77.7% of the control group, and grade 3/4 AEs occurred in 47.4% versus 25.2%, respectively.
It was concluded that this study met its primary objective, demonstrating significantly prolonged Overall Survival with first-line maintenance BAVENCIO® plus BSC compared with BSC alone, in all patients with advanced Urothelial Carcinoma, and should therefore be the new first-line standard of care in this patient group.
Maintenance avelumab + best supportive care (BSC) versus BSC alone after platinum-based first-line (1L) chemotherapy in advanced urothelial carcinoma (UC): JAVELIN Bladder 100 phase III interim analysis. Powles T, Park SH, Voog E, et al. J Clin Oncol 38: 2020 (suppl; abstr LBA1)
BAVENCIO® (Avelumab)
The FDA on June 30, 2020 approved BAVENCIO® for maintenance treatment of patients with locally advanced or metastatic Urothelial Carcinoma (UC) that has not progressed with first-line Platinum-containing chemotherapy. BAVENCIO® is a product of EMD Serono, Inc.
JELMYTO® (Mitomycin)
The FDA on April 15, 2020 approved JELMYTO® for adult patients with low-grade upper tract urothelial cancer. JELMYTO® is a product of UroGen Pharma.
FDA Approves KEYTRUDA® for BCG-Unresponsive, High-Risk Non-Muscle Invasive Bladder Cancer
SUMMARY: The FDA on January 8, 2020, approved KEYTRUDA® (Pembrolizumab) for the treatment of patients with Bacillus Calmette-Guerin (BCG)-unresponsive, high-risk, Non-Muscle Invasive Bladder Cancer (NMIBC) with Carcinoma In Situ (CIS) with or without papillary tumors, who are ineligible for or have elected not to undergo cystectomy.
The American Cancer Society estimates that for 2020, about 81,400 new cases of bladder cancer will be diagnosed in the US and about 17,980 patients will die of the disease. Bladder cancer is the fourth most common cancer in men, but is less common in women and the average age at the time of diagnosis is 73. Approximately 50% of all bladder cancers are non-invasive or in situ cancers. Patients with high-risk, Non-Muscle Invasive Bladder Cancer that has become unresponsive to BCG treatment, are often given the treatment option of radical cystectomy, which includes removing the entire urinary bladder and a prostatectomy for men or total hysterectomy in women. While highly curative, this surgical procedure carries substantial risk for morbidity and mortality, and can negatively impact patient’s quality of life. Further, a significant proportion of patients are medically ineligible for a radical cystectomy, and even if eligible, refuse surgery and opt for other less effective treatments, which could compromise outcomes.
KEYTRUDA® is a fully humanized, Immunoglobulin G4, anti-PD-1, monoclonal antibody, that binds to the PD-1 receptor and blocks its interaction with ligands PD-L1 and PD-L2. By doing so, it unleashes the tumor-specific effector T cells, and is thereby able to undo PD-1 pathway-mediated inhibition of the immune response. KEYTRUDA® is presently approved by the FDA for the treatment of patients with locally advanced or metastatic Urothelial carcinoma who are not eligible for Cisplatin-containing chemotherapy or for those with disease progression during or following platinum-containing chemotherapy, based on its durable antitumor activity in this patient group. Upregulation of the PD-1 pathway has been observed in BCG-resistant NMIBC, suggesting that KEYTRUDA® may be of benefit in this group of patients.
This new FDA approval for KEYTRUDA® was based on the KEYNOTE-057 study, which is a multicenter, single-arm trial that enrolled 148 patients with high-risk NMIBC, of whom 96 patients had BCG-unresponsive CIS with or without papillary tumors. BCG-unresponsive high-risk Non-Muscle Invasive Bladder Cancer was defined as persistent disease despite adequate BCG therapy, disease recurrence after an initial tumor-free state following adequate BCG therapy, or T1 disease following a single induction course of BCG. Eligible patients had received adequate BCG therapy and were unable/unwilling to undergo radical cystectomy. All patients had undergone TransUrethral Resection of Bladder Tumor (TURBT) to remove resectable disease. Patients with residual Carcinoma In Situ, not amenable to complete resection were permitted. Patients received KEYTRUDA® 200 mg every 3 weeks until unacceptable toxicity, persistent or recurrent high-risk NMIBC or progressive disease, or up to 24 months of therapy without disease progression. The median age was 73 years and the median number of prior BCG instillations was 12. More than half of patients (56.9%) had a PD-L1 Combined Positive Score (CPS) of less than 10, and most patients in this analysis had refused prior cystectomy. The Primary end point was Complete Response Rate (CRR) as defined by negative results for cystoscopy with TURBT/biopsies as applicable, urine cytology, and CT Urography imaging. Secondary end points included Duration of Response and Safety.
At a median follow up was 28 months the Complete Response Rate was 41% and the median Duration of Response was 16.2 months. Forty-six percent (46%) of responding patients experienced a Complete Response lasting at least 12 months. The most frequent adverse reactions were fatigue, diarrhea, rash, pruritis, musculoskeletal pain, peripheral edema and hypothyroidism.
It was concluded from this study that KEYTRUDA® had encouraging activity in bladder cancer patients, with high-risk, BCG-unresponsive Carcinoma in Situ, with or without papillary tumors. The authors added that this study demonstrates that immune activation with systemically administered treatment can result in local activity in the bladder, as well as long-term durable remissions of cancer.
Keynote 057: Phase II trial of Pembrolizumab (pembro) for patients (pts) with high-risk (HR) nonmuscle invasive bladder cancer (NMIBC) unresponsive to bacillus calmette-guérin (BCG). Balar AV, Kulkarni GS, Uchio EM, et al. J Clin Oncol 37, 2019 (suppl 7S; abstr 350)
KEYTRUDA® (Pembrolizumab)
he FDA on January 8, 2020 approved KEYTRUDA® for the treatment of patients with Bacillus Calmette-Guerin (BCG)-unresponsive, high-risk, Non-Muscle Invasive Bladder Cancer (NMIBC) with Carcinoma In Situ (CIS), with or without papillary tumors, who are ineligible for or have elected not to undergo cystectomy. KEYTRUDA® is a product of Merck & Co. Inc.
PADCEV® (Enfortumab vedotin-ejfv)
The FDA on December 18, 2019 granted accelerated approval to PADCEV® for adult patients with locally advanced or metastatic urothelial cancer who have previously received a Programmed Death receptor-1 (PD-1) or Programmed Death-Ligand 1 (PD-L1) inhibitor, and a Platinum-containing chemotherapy in the neoadjuvant/adjuvant, locally advanced or metastatic setting. PADCEV® is a product of Astellas Pharma US, Inc.
FDA Grants Accelerated Approval to PADCEV® for Metastatic Urothelial Cancer
SUMMARY: The FDA on December 18, 2019, granted accelerated approval to PADCEV® (Enfortumab vedotin-ejfv), for adult patients with locally advanced or metastatic urothelial cancer who have previously received a Programmed Death receptor-1 (PD-1) or Programmed Death-Ligand1 (PD-L1) inhibitor, and a Platinum-containing chemotherapy in the neoadjuvant/adjuvant, locally advanced or metastatic setting. The American Cancer Society estimates that in 2019, approximately 80,470 new cases of Bladder Cancer will be diagnosed and 17,670 patients will die of the disease. Patients with urothelial carcinoma are currently treated in the first line setting with a Platinum based chemotherapy regimen and a Check Point Inhibitor (PD-1 or PD-L1 inhibitor) in the second line setting. Treatment options for patients who progress after first and second line therapies are limited, with poor outcomes. The response rates with standard chemotherapy in this patient population, is about 10%.
PADCEV® is an Antibody-Drug Conjugate (ADC) that targets Nectin-4, a cell adhesion molecule highly expressed in urothelial cancers and other solid tumors. Following binding to Nectin-4 on the cell surface, PADCEV® becomes internalized and is processed by lysosomes, with the liberation of its cytotoxic payload, Monomethyl auristatin E, which in turn disrupts microtubule assembly, leading to cell cycle arrest and apoptosis. In a Phase I dose-finding study of PADCEV®, the Objective Response Rate (ORR) was 42% among patients with advanced urothelial cancer, who previously received treatment with a PD-1/PD-L1 inhibitor.
This FDA approval was based on the results from the pivotal Phase II EV-201 study, which is an open-label, single-arm, multicenter trial in which 125 patients with locally advanced or metastatic urothelial cancer who received prior treatment with a PD-1 or PD-L1 inhibitor and Platinum-based chemotherapy were enrolled. Patients received PADCEV® 1.25 mg/kg on days 1, 8, and 15 of a 28-day cycle, until disease progression or unacceptable toxicity. The median age was 69 years. The Primary endpoint was ORR as assessed by blinded Independent Central Review. Secondary endpoints included Duration of Response, Progression Free Survival (PFS), Overall Survival (OS), Safety and Tolerability.
The ORR was 44%, with 12% Complete Responses and 32% Partial Responses. Overall, 84% of evaluable patients showed some degree of tumor shrinkage. The responses were noted at a median of 1.8 months after treatment initiation and the median Duration of Response was 7.6 months. These objective responses were seen in all patient subgroups evaluated, including those with poor prognostic features. The median PFS was 5.8 months, and the median Overall Survival was 11.7 months. The most common adverse reactions were fatigue, alopecia, decreased appetite and peripheral neuropathy. Blood glucose levels should be monitored closely in patients with, or at risk, for diabetes mellitus or hyperglycemia.
It was concluded from this study that treatment with PADCEV® demonstrated clinically meaningful Objective Response Rate, in patients with advanced metastatic urothelial cancer, who received prior treatment with a PD-1 or PD-L1 inhibitor and Platinum-based chemotherapy, thus fulfilling an unmet need. PADCEV® is the first Nectin-4-directed Antibody-Drug Conjugate to receive FDA approval, and a Phase III study is underway comparing PADCEV® against standard single-agent chemotherapy, in patients with advanced, previously treated metastatic urothelial cancer. EV-201: Results of enfortumab vedotin monotherapy for locally advanced or metastatic urothelial cancer previously treated with platinum and immune checkpoint inhibitors. Petrylak DP, Balar AV, O’Donnell PH, et al. DOI: 10.1200/JCO.2019.37.18_suppl.LBA4505 Journal of Clinical Oncology 37, no. 18_suppl (June 20, 2019) 4505-4505.
FDA Approves BALVERSA® for Metastatic Urothelial Carcinoma
SUMMARY: The FDA on April 12, 2019 granted accelerated approval to BALVERSA® (Erdafitinib) for patients with locally advanced or metastatic Urothelial Carcinoma, with susceptible FGFR3 or FGFR2 genetic alterations,that has progressed during or following platinum-containing chemotherapy, including within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy. Patients should be selected for therapy based on an FDA-approved companion diagnostic for BALVERSA®. The FDA also simultaneously approved the THERASCREEN® FGFR RGQ RT-PCR Kit, developed by QIAGEN, for use as a companion diagnostic for this therapeutic indication.
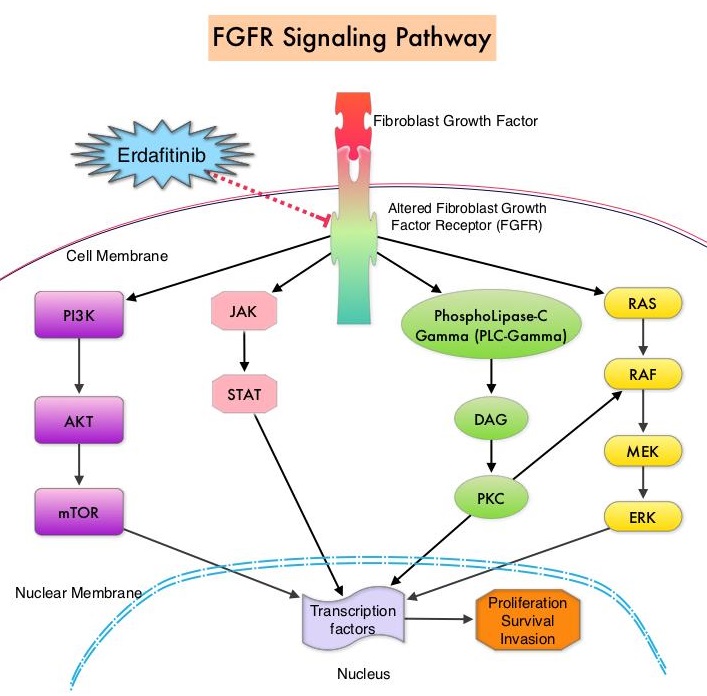 FGFRs are a family of Receptor Tyrosine Kinases, which may be upregulated in a variety of malignancies. The Fibroblast Growth Factor/Fibroblast Growth Factor Receptor (FGF/FGFR) signaling pathway regulates embryogenesis, adult tissue homeostasis, angiogenesis and wound repair, and is also pivotal in cell functions, including proliferation, differentiation, apoptosis and migration. Deregulated FGF/FGFR activations have been associated with developmental disorders and cancer progression. Following binding with a ligand, FGFRs activate downstream signaling pathways such as the Mitogen Activated Protein Kinase (MAPK), Signal Transducer and Activator of Transcription (STAT), the PhosphoInositide-3-Kinase (PI3K)/Akt pathways, and PLC-DAG-PKC pathway. FGFR isoforms have been shown to result in oncogenic FGFR signaling, which in turn promotes tumorigenesis. FGFR3 mutations have been described in approximately 75% of low-grade papillary bladder cancers, and FGFR3 overexpression has been noted in 42% of muscle-invasive bladder cancers. FGFR1 amplification has also been found in 3% of urinary bladder cancers. Patients with FGFR alterations have poor outcomes when treated with available therapies and these alterations occur in 20% of patients with metastatic Urothelial Carcinoma.
FGFRs are a family of Receptor Tyrosine Kinases, which may be upregulated in a variety of malignancies. The Fibroblast Growth Factor/Fibroblast Growth Factor Receptor (FGF/FGFR) signaling pathway regulates embryogenesis, adult tissue homeostasis, angiogenesis and wound repair, and is also pivotal in cell functions, including proliferation, differentiation, apoptosis and migration. Deregulated FGF/FGFR activations have been associated with developmental disorders and cancer progression. Following binding with a ligand, FGFRs activate downstream signaling pathways such as the Mitogen Activated Protein Kinase (MAPK), Signal Transducer and Activator of Transcription (STAT), the PhosphoInositide-3-Kinase (PI3K)/Akt pathways, and PLC-DAG-PKC pathway. FGFR isoforms have been shown to result in oncogenic FGFR signaling, which in turn promotes tumorigenesis. FGFR3 mutations have been described in approximately 75% of low-grade papillary bladder cancers, and FGFR3 overexpression has been noted in 42% of muscle-invasive bladder cancers. FGFR1 amplification has also been found in 3% of urinary bladder cancers. Patients with FGFR alterations have poor outcomes when treated with available therapies and these alterations occur in 20% of patients with metastatic Urothelial Carcinoma.
BALVERSA® (Erdafitinib) is a once-daily, oral, pan-Fibroblast Growth Factor Receptor (FGFR) Tyrosine Kinase Inhibitor. The approval of BALVERSA® was based on data from a cohort of 87 patients, enrolled in Study BLC2001, which is a multicenter, open-label, single-arm trial. Enrolled patients had locally advanced or metastatic Urothelial Carcinoma that had progressed during, or following at least one prior chemotherapy regimen, and had FGFR genomic alterations such as FGFR3 gene mutations or FGFR2 or FGFR3 gene fusions. Ten percent of patients were chemo naïve, 47% percent of patients had received two or more prior lines of therapy and 80% of patients had visceral metastases. Approximately 97% patients had prior Platinum based therapy and 24% of patients had received anti–PD-1/PD-L1 treatment. The median patient age was 67 years. Patients received BALVERSA® at a starting dose of 8 mg PO once daily. Patients whose serum phosphate levels were below the target of 5.5 mg/dL between days 14 and 17 (41% of the patients) had their dose increased to 9 mg once daily. Treatment was continued until disease progression or unacceptable toxicity. The Primary end point was Objective Response Rate (ORR).
The ORR was 32.2%, with Complete Responses in 2.3% and Partial Responses in 29.9%. Median response duration was 5.4 months. Responding patients included those patients who had previously not responded to anti PD-L1 or PD-1 treatment. The most common adverse reactions were increased serum phosphate, stomatitis, fatigue, increased serum creatinine, diarrhea, onycholysis, increased liver function studies and hyponatremia.
The authors concluded that treatment with BALVERSA® resulted in high Response Rates among patients with chemorefractory metastatic Urothelial Carcinoma with FGFR genomic alterations. BALVERSA® is the first approved personalized treatment, targeting susceptible FGFR genetic alterations, fulfilling an unmet need for these poor prognosis patients. First results from the primary analysis population of the phase 2 study of erdafitinib (ERDA; JNJ-42756493) in patients (pts) with metastatic or unresectable urothelial carcinoma (mUC) and FGFR alterations (FGFRalt). Siefker-Radtke AO, Necchi A, Park SH, et al. J Clin Oncol 36, 2018 (suppl; abstr 4503)
