SUMMARY: Lung cancer is the second most common cancer in both men and women and accounts for about 13% of all new cancers and 21% of all cancer deaths. The American Cancer Society estimates that for 2023, about 238,340 new cases of lung cancer will be diagnosed and 127,070 patients will die of the disease. Lung cancer is the leading cause of cancer-related mortality in the United States. Non-Small Cell Lung Cancer (NSCLC) accounts for approximately 85% of all lung cancers. Of the three main subtypes of NSCLC, 30% are Squamous Cell Carcinomas (SCC), 40% are Adenocarcinomas and 10% are Large Cell Carcinomas. With changes in the cigarette composition and decline in tobacco consumption over the past several decades, Adenocarcinoma now is the most frequent histologic subtype of lung cancer.
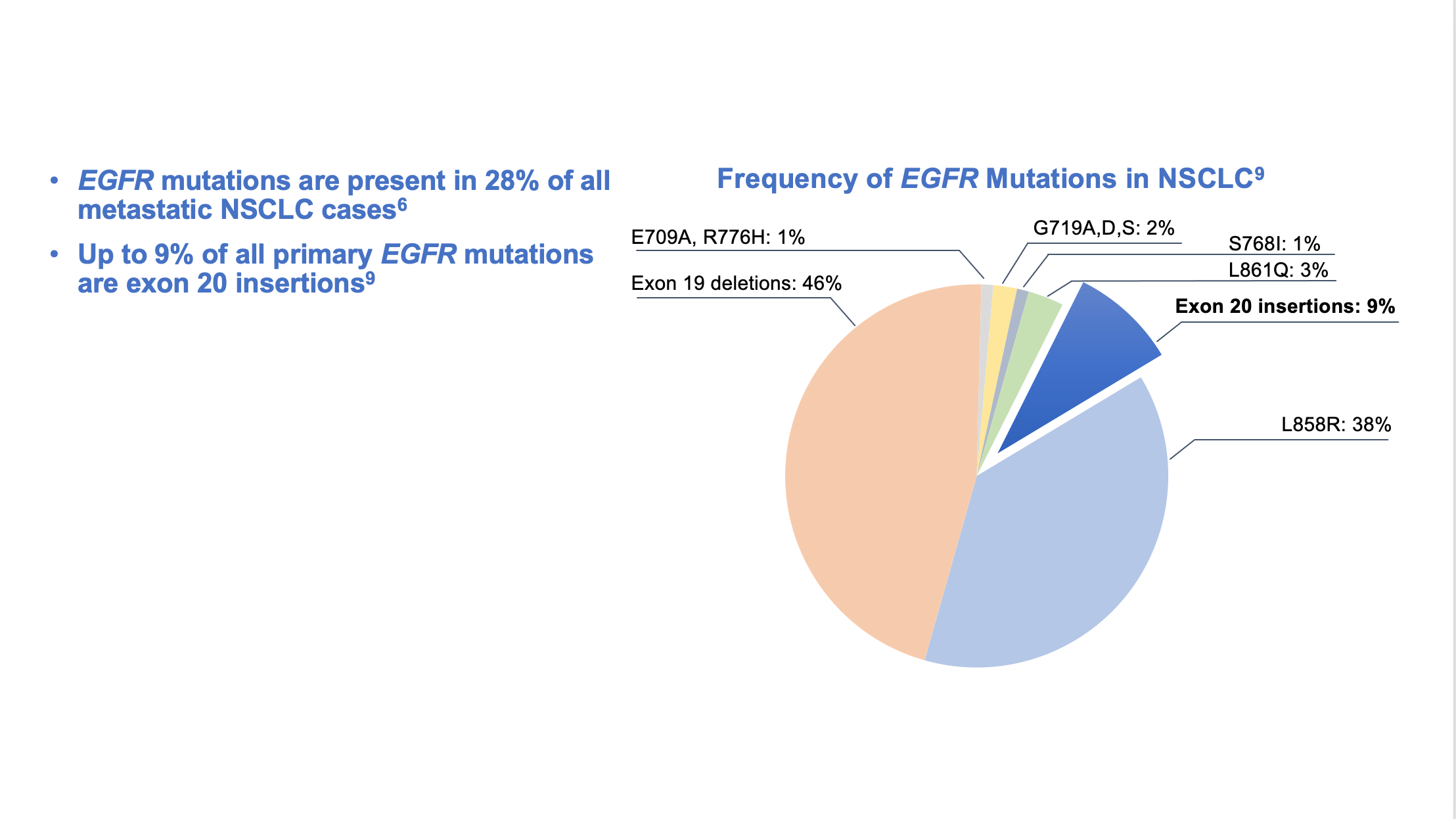
Approximately 10-15% of Caucasian patients and 35-50% of Asian patients with Adenocarcinomas, harbor activating EGFR (Epidermal Growth Factor Receptor) mutations and 90% of these mutations are either Exon 19 deletions or L858R substitution mutation in Exon 21. Approximately 25% of patients with EGFR mutated NSCLC have brain metastases at diagnosis, increasing to approximately 40% within two years of diagnosis. The presence of brain metastases often reduces median survival to less than eight months. EGFR-Tyrosine Kinase Inhibitors (TKIs) such as TARCEVA® (Erlotinib), IRESSA® (Gefitinib) and GILOTRIF® (Afatinib), have demonstrated a 60-70% response rate as monotherapy when administered as first line treatment, in patients with metastatic NSCLC, who harbor the sensitizing EGFR mutations. However, majority of these patients experience disease progression within 9-14 months. This resistance to frontline EGFR TKI therapy has been attributed to the most common, acquired T790M “gatekeeper” point mutation in EGFR, identified in 50-60% of patients.
TAGRISSO® (Osimertinib) is a highly selective third-generation Epidermal Growth Factor Receptor (EGFR) TKI presently approved by the FDA, for the first-line treatment of patients with metastatic NSCLC, whose tumors have Exon 19 deletions or Exon 21 L858R mutations, as well as treatment of patients with metastatic EGFR T790M mutation-positive NSCLC, whose disease has progressed on or after EGFR-TKI therapy. Further, TAGRISSO® has higher CNS penetration and is therefore able to induce responses in 70-90% of patients with brain metastases. Among patients with metastatic, EGFR-mutant NSCLC, first-line treatment with TAGRISSO® significantly improved median Overall Survival, compared with TARCEVA® and IRESSA®, and should therefore be considered the preferred regimen.
Surgical resection is the primary treatment for approximately 30% of patients with NSCLC who present with early Stage (I–IIIA) disease. These patients are often treated with platinum-based adjuvant chemotherapy to decrease the risk of recurrence. Nonetheless, 45-75% of these patients develop recurrent disease. There is therefore an unmet need for this patient population.
ADAURA is a global, double-blind, randomized Phase III study, which assessed the efficacy and safety of TAGRISSO® versus placebo in patients with Stage IB–IIIA EGFR mutated NSCLC, after complete tumor resection and adjuvant chemotherapy, when indicated. In this study, 682 patients with completely resected Stage IB, II, IIIA NSCLC, with or without postoperative adjuvant chemotherapy, were randomly assigned 1:1 to receive either TAGRISSO® 80 mg orally once daily (N=339) or placebo (N=343) once daily, for up to 3 years. Eligible patients had an ECOG Performance Status of 0 or 1, with confirmed EGFR mutations (Exon 19del or L858R). Treatment groups were well balanced and patients were stratified by Stage (IB/II/IIIA), mutation type (Exon 19del/L858R), and race (Asian/non-Asian). Most patients with Stage II to IIIA disease (76%) and approximately a quarter of the patients with Stage IB disease (26%) received adjuvant platinum-based chemotherapy. The Primary endpoint was Disease Free Survival (DFS) in Stage II–IIIA patients. Secondary endpoints included DFS in the overall population of patients with Stage IB to IIIA disease, Overall Survival (OS) and Safety. Following Independent Data Monitoring Committee recommendation, the trial was unblinded early, due to efficacy.
The FDA approved TAGRISSO® for use as adjuvant treatment in late 2020 based on the primary analysis data demonstrating that in the patients with Stage II/IIIA disease, the DFS had not been reached with TAGRISSO® versus 19.6 months with placebo (HR=0.17; P<0.001). This was equal to an 83% reduction in the risk of recurrence or death, indicating a significantly longer DFS among patients in the TAGRISSO® group, compared to those in the placebo group. The 2-year DFS rate in this patient group with TAGRISSO® was 90% versus 44% with placebo. In the overall population, which included Stage IB to IIIA disease, the median DFS was not reached with TAGRISSO® versus 27.5 months with placebo (HR=0.20; P<0.001). This Hazard Ratio equaled to an 80% reduction in the risk of disease recurrence or death among patients in the TAGRISSO® group compared to those in the placebo group. The 2-year DFS rate in the overall population was 89% with TAGRISSO® versus 52% with placebo. Updated data presented at the 2022 ESMO Congress showed that at a median follow up of 44.2 months, the DFS with TAGRISSO® was still robust at 77% in patients with Stage II/IIIA disease and 73% in the overall Stage IB-IIIA population.
The researchers herein reported the planned final Overall Survival (OS) analysis from ADAURA. Adjuvant TAGRISSO® significantly improved OS compared to placebo and reduced the risk of death by 51% compared to placebo in both Stages II-IIIA (HR for OS=0.49; P=0.0004), and in the overall Stages IB-IIIA trial population (HR=0.49; P<0.0001). This survival benefits with TAGRISSO® was seen, regardless of whether prior adjuvant chemotherapy was received. The 5-year OS rate was 88% in the TAGRISSO® group and 78% in the placebo group. Median OS was not reached in either population or treatment group. The safety profile with adjuvant TAGRISSO® was consistent with that in the primary analysis.
It was concluded that adjuvant TAGRISSO® demonstrated an unprecedented, highly statistically significant and clinically meaningful Overall Survival benefit in patients with EGFR mutated Stage IB–IIIA NSCLC after complete tumor resection, with or without adjuvant chemotherapy. The authors added that ADAURA is the first global Phase III study to demonstrate a statistically significant Disease Free Survival and Overall Survival benefit with targeted treatment for this patient group, reinforcing the importance of testing for biomarkers at the time of diagnosis and before starting therapy.
Overall Survival with Osimertinib in Resected EGFR-Mutated NSCLC. Tsuboi M, Herbst RS, John T, et al., for the ADAURA Investigators. June 4, 2023. DOI: 10.1056/NEJMoa2304594