Written By: Debra Patt, MD, PhD, MBA
In the golden age of oncology, many patients can now live with cancer as a chronic disease. Understanding how to optimally block cancer growth and how cancers develop mechanisms of resistance is critical to improving therapy.
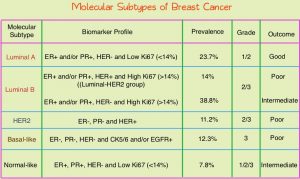
For most patients with advanced breast cancer, estrogen blockade is the mainstay of early cancer treatments. Optimizing estrogen blockade in combination with other targets has dramatically improved progression-free and overall survival in patients with advanced breast cancer. Optimizing endocrine blockade in patients with ER+ advanced breast cancer is not only an effective therapy that improves outcomes, but also delays other systemic therapy, like chemotherapy, which have a toxicity profile that is typically more severe than endocrine therapy alone. By delaying chemotherapy with effective endocrine therapy, patients can enjoy longer disease-free intervals and maintain a high quality of life. While estrogen-positive breast cancer can be targeted by many estrogen-targeted therapies, resistance to aromatase inhibition through the development of ESR1 mutations is an important mechanism of resistance that contributes to cancer progression via the endocrine blockade.1
As we continue to make progress in cancer care, becoming familiar with new therapies is critical. This article will review elacestrant, approved by the Food and Drug Administration (FDA) in January 2023 for patients with estrogen receptor-positive (ER+) advanced breast cancer with ESR1 mutations after at least one line of endocrine therapy.
The superior response among patients with ESR1 mutations led to FDA approval among patients with ESR1 mutations who had received at least one line of endocrine therapy. Because ESR1 mutation status is central to FDA approval and the basis of many coverage determinations from payers, assessing ESR1 mutation status accurately is an important aspect of treatment. ESR1 mutations can develop in patients with ER+ advanced breast cancer and can change over time. In patients with treatment naïve early-stage breast cancer, de novo ESR1 mutations are relatively rare, but as patients are exposed to therapy, ESR1 mutations are acquired, making them a common mechanism of resistance in patients with metastatic disease.2 Because mutations develop over time with the evolutionary pressure of therapy, a patient’s ESR1 mutation status, when they are initially diagnosed with ER+ metastatic disease, can later change after exposure to aromatase inhibition. If analysis for ESR1 mutations is conducted early in a patient’s treatment and is found negative, resistance may emerge and only be demonstrated with subsequent molecular testing. There is evidence that blood-based serial testing may be a useful way to identify patients who are eligible for treatment.3 In January 2023, Guardant Health, through the Guardant 360 CDx, was approved by the FDA as a tool to test the blood for ESR1 mutations to assess for eligibility for elacestrant. By using sequential serologic testing, patients can have an assessment of molecular characteristics without undergoing additional biopsy. Because such a small number of patients have ESR1 mutations when they are treatment naïve, but it becomes much more likely through the course of a patient’s disease, repeat testing is the primary way to assess if ESR1 mutations have evolved over time, and can be conducted via plasma assessment.
Elacestrant works by binding estrogen receptor alpha and acting as a Selective Estrogen Receptor Down regulator (SERD), allowing degradation of the estrogen receptor. The FDA approved elacestrant in 2023 based on the reporting of the phase III EMERALD trial showing that patients with ER-positive and HER2 negative advanced breast cancer who had had one to two lines of endocrine therapy, pretreatment with a cyclin-dependent kinase 4/6 inhibitor, and not more than one line of chemotherapy, achieved a significant progression-free survival advantage when treated with elacestrant in comparison to other therapy.4 The population was further stratified as the whole population vs. just those with ESR1 mutations. In the entire population treated with elacestrant, PFS was prolonged (HR=0.70; 95% CI=0.55-0.88), and the results were more striking in those with ESR1 mutations (HR=0.55; 95% CI=0.39-0.77). In this group of pretreated patients with advanced breast cancer, ESR1 mutations were detected in 47.8% of patients. The progression-free survival of patients in the EMERALD trial was 3.8 months among patients receiving elacestrant in comparison to 1.9 months for other commonly prescribed endocrine therapies.
Elecestrant was well tolerated with treatment-related grade 3/4 adverse events in 7.2% of patients receiving elecestrant in comparison to 3.1% in patients receiving standard-of-care. Nausea was the most common side effect occurring to any extent in 35% of patients receiving elecestrant (though grade 3 was 2.5% and grade 4 was 0.9%) in comparison to 18.8% in patients who were receiving standard-of-care treatment. Other common side effects include abdominal pain, vomiting, diarrhea, constipation, elevation of liver function tests, cytopenias, hyponatremia, and fatigue. To mitigate side effects, it can help to take the medication with food, administer it at the same time each day, and use supportive anti-nausea and anti-diarrheal guidance upfront, in addition to dose reductions as appropriate.
In our modern era of cancer treatment, optimizing the use of incremental therapy can benefit patients. Making sure we consider ESR1 mutations in patients with ER+ advanced breast cancer, offer appropriate testing as patients are exposed to different treatments, and anticipate and mitigate side effects as appropriate will help us manage patients with ER+ advanced breast cancer optimally.
References
1) Brett, J.O., Spring, L.M., Bardia, A. et al. ESR1 mutation as an emerging clinical biomarker in metastatic hormone receptor-positive breast cancer. Breast Cancer Res 23, 85 (2021). https://doi.org/10.1186/s13058-021-01462-3.
2) Kinslow CJ, Tang A, Chaudhary KR, Cheng SK. Prevalence of Estrogen Receptor Alpha (ESR1) Somatic Mutations in Breast Cancer. JNCI Cancer Spectr. 2022 Sep 1;6(5):pkac060. doi: 10.1093/jncics/pkac060. PMID: 35959983; PMCID: PMC9438742.
3) Sundaresan TK, Dubash TD, Zheng Z, Bardia A, Wittner BS, Aceto N, Silva EJ, Fox DB, Liebers M, Kapur R, Iafrate J, Toner M, Maheswaran S, Haber DA. Evaluation of endocrine resistance using ESR1 genotyping of circulating tumor cells and plasma DNA. Breast Cancer Res Treat. 2021 Jul;188(1):43-52. doi: 10.1007/s10549-021-06270-z. Epub 2021 Jun 8. PMID: 34101078; PMCID: PMC8667563.
4) Bidard FC, Kaklamani VG, Neven P, Streich G, Montero AJ, Forget F, Mouret-Reynier MA, Sohn JH, Taylor D, Harnden KK, Khong H, Kocsis J, Dalenc F, Dillon PM, Babu S, Waters S, Deleu I, García Sáenz JA, Bria E, Cazzaniga M, Lu J, Aftimos P, Cortés J, Liu S, Tonini G, Laurent D, Habboubi N, Conlan MG, Bardia A. Elacestrant (oral selective estrogen receptor degrader) Versus Standard Endocrine Therapy for Estrogen Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer: Results From the Randomized Phase III EMERALD Trial. J Clin Oncol. 2022 Oct 1;40(28):3246-3256. doi: 10.1200/JCO.22.00338. Epub 2022 May 18. Erratum in: J Clin Oncol. 2023 Aug 10;41(23):3962. PMID: 35584336; PMCID: PMC9553388.