SUMMARY: The SARS-CoV-2 Coronavirus (COVID-19) induced pandemic first identified in December 2019 in Wuhan, China, has contributed to significant mortality and morbidity in the US, and the number of infected cases continue to exponentially increase worldwide. Majority of the patients present with treatment-resistant pyrexia and respiratory insufficiency, with some of these patients progressing to a more severe systemic disease and multiple organ dysfunction.
One of the most important and significant poor prognostic features in patients with COVID-19 is the development of coagulopathy, which is associated with an increased risk of death. The coagulation changes seen suggest the presence of a hypercoagulable state that can potentially increase the risk of thromboembolic complications. The coagulation abnormalities mimic other systemic coagulopathies associated with severe infections, such as Disseminated Intravascular Coagulation (DIC) or Thrombotic MicroAngiopathy (TMA), but the features are distinct in that, with DIC associated with sepsis, thrombocytopenia is usually more profound, and D-dimer concentrations do not reach the high values as seen among patients with COVID-19. COVID-19 infection related coagulopathy can also be associated with increased Lactate DeHydrogenase (LDH), and in some patients strikingly high ferritin levels, reminiscent of findings in TMA.
Severe COVID-19 infection is characterized by high concentrations of proinflammatory cytokines and chemokines such as Tumor Necrosis Factor-α (TNF-α) and interleukins including IL-1 and IL-6. IL-6 can induce tissue factor expression on mononuclear cells, initiating coagulation activation and thrombin generation, whereas TNF-α and IL-1 suppress endogenous anticoagulant pathways.
The International Society of Thrombosis and Haemostasis (ISTH) in this publication provided an interim guidance, with the aim to help Health Care Specialists risk stratify patients admitted with COVID -19, and manage coagulopathy, which may develop in some of these patients, utilizing easily available laboratory parameters. Based on the currently available literature, majority of the patients with COVID-19, present with severe pneumonia and respiratory failure. Lymphopenia is a common hematological abnormality. The interim guidance statement by the ISTH on the management of coagulopathy is based on evolving clinical knowledge and better understanding of the pathogenesis of COVID-19.
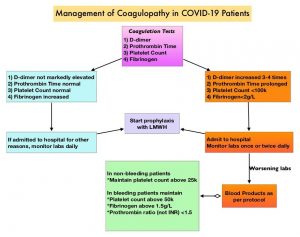
1) Initial evaluation of COVID-19 patients should include measurement of D-dimers, Prothrombin Time, Platelet count and Fibrinogen levels.
2) Higher D-dimer levels on admission, has been reported in patients with severe COVID-19 illness, and is one of the most important predictors of mortality.
3) Modest prolongation of Prothrombin Time (15.5 seconds) has been reported at admission, in the non-survivors. Subtle changes in the PT will not be picked up if the PT is reported as International Normalized Ratio (INR). It should be noted that INR is not the same as PT ratio.
4) Thrombocytopenia at the time of admission may be, but is not a consistent prognosticator and platelet count of less than 100 × 109/L may only be seen in 5% of patients
5) Fibrinogen should be regularly monitored in COVID-19 patients, as non-survivors with severe illness usually develop Disseminated Intravascular Coagulation around day 4, with significant worsening noted at days 10 and 14.
6) In the absence of any contraindications such as active bleeding and platelet count less than 25 × 109/L, prophylactic dose Low Molecular Weight Heparin (LMWH) should be considered in all patients who require hospital admission for COVID‐19 infection, including those who are non‐critically ill, to protect patients against septic-like coagulopathy and Venous ThromboEmbolism (VTE). The anti‐inflammatory properties of LMWH may be an added benefit in COVID infection where pro‐inflammatory cytokines are markedly raised.
7) Abnormal PT or aPTT is not a contraindication for pharmacological thromboprophylaxis as Lupus-like inhibitors have been reported in some patients with COVID-19, and may be the reason for aPTT prolongation.
8) In COVID-19 patients already on anticoagulation for VTE or Atrial Fibrillation, therapeutic doses of anticoagulant therapy should be continued, but may need to be held if the platelet count is less than 30-50 x 109/L or if the fibrinogen is less than 1.0 g/L.
9) Bleeding is rare in the setting of COVID‐19 and if present should be managed by maintaining platelet counts >50×109/L (>20×109/L goal in non-bleeding patients), maintaining fibrinogen levels at >2.0 g/L, and the Prothrombin ratio at <1.5.
ISTH interim guidance on recognition and management of coagulopathy in COVID‐19. Thachil J, Tang N, Gando S, et al. J Thromb Haemost 2020 Mar 25; [e-pub]. (https://doi.org/10.1111/JTH.14810)

